Postpartum Recovery Guide: The Fourth Trimester Explained
Nobody told you this part would be harder than pregnancy. Here's what actually happens to your body in the 12 weeks after birth—and what's normal vs. when to call your doctor.
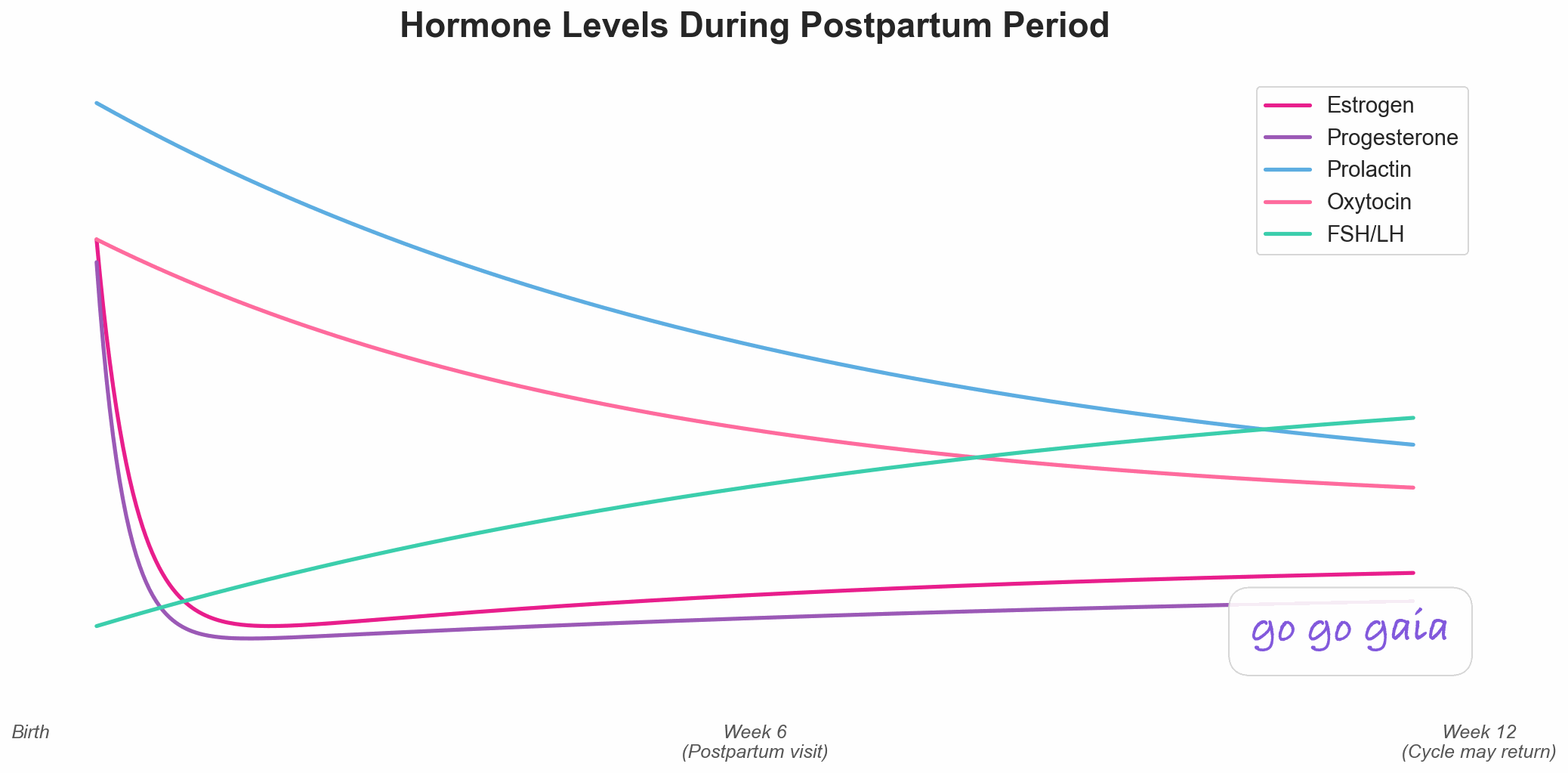
The dramatic hormone drop after birth—one of the largest hormonal shifts in human physiology
Medical Disclaimer
This article is for educational and informational purposes only and does not constitute medical advice. The information provided is based on general wellness principles and should not replace consultation with qualified healthcare professionals. Always consult your OB-GYN or healthcare provider about postpartum recovery, especially if you have complications, underlying health conditions, or concerns about your physical or mental health. If you're experiencing severe depression, anxiety, or thoughts of self-harm, please call 988 (Suicide & Crisis Lifeline) or seek immediate professional help. Individual recovery experiences vary, and what works for one person may not work for another.
You survived labor. The baby is here. Everyone's congratulating you. And you're sitting there, exhausted, bleeding, covered in sweat at 3 AM, thinking: "When does this get easier?"
Welcome to the fourth trimester. The 12 weeks after birth that nobody prepares you for.
Your hormones just crashed harder than they've ever crashed in your life. Your body is healing from what's essentially a major medical event. You're not sleeping. Your emotions are all over the place. And every online mom forum insists this is "normal," but nobody's explaining what normal actually means or when to worry.
Here's what's really happening—and what you need to know to get through it.
What Is the Fourth Trimester?
The fourth trimester is weeks 0-12 after birth. It's when your body transitions from pregnancy back to... not pregnant. But that transition isn't instant, and it's not smooth.
During pregnancy, your hormones spent 40 weeks climbing to levels 10 to 100 times higher than normal.[1] Estrogen, progesterone, HCG—all at peak levels to support the baby.
Then you deliver the placenta. And within hours, those hormones drop. Not gradually. Not slowly. They crash.
This is one of the most dramatic hormonal shifts in human physiology.[1] Bigger than puberty. Bigger than menopause. And your body has to adjust while you're also recovering physically, not sleeping, and learning to keep a tiny human alive.
That's the fourth trimester. And it's hard.
The Hormone Crash: What's Happening
Estrogen and Progesterone Plummet
During pregnancy, the placenta produces massive amounts of estrogen and progesterone to maintain the pregnancy and prepare your body for birth and breastfeeding.
What happens after birth:
- Estrogen and progesterone drop by approximately 90% within the first 24 hours after delivery[1]
- They continue declining over the next 5-7 days, reaching near-baseline levels by week 1-2
- This crash is steeper and faster than any other hormonal change you'll experience
Why this matters:
Estrogen and progesterone affect mood regulation, sleep quality, temperature regulation, and energy levels. When they crash, you get:
- Night sweats: Your body is adjusting its thermostat without progesterone's warming effect
- Mood swings: Estrogen helps regulate serotonin.[2] Less estrogen = more emotional volatility
- Fatigue: Beyond just sleep deprivation—your body is metabolically adjusting
- Brain fog: Estrogen affects cognition and memory
This is not "just hormones." This is a massive physiological event. Telling someone "it's just hormones" minimizes how real and intense these changes are. Your body just went through something enormous, and these symptoms are your body adjusting.
Breastfeeding Hormones Rise (If You're Nursing)
If you're breastfeeding, two new hormones take over:
Prolactin:
- Stimulates milk production
- Rises every time you nurse or pump
- Suppresses ovulation (nature's way of spacing pregnancies)
- Can affect mood and energy—some people feel calm, others feel more anxious
Oxytocin:
- Triggers milk letdown reflex
- Released in pulses during breastfeeding
- Also causes uterine contractions (those "afterpains" during nursing)
- Promotes bonding (but doesn't guarantee instant bonding—that's a myth)
These hormones help with milk production but also delay the return of your menstrual cycle. More on that later.
Physical Recovery: What to Expect Week by Week
Weeks 0-2: The Hardest Phase
What's happening:
- Lochia (postpartum bleeding): Heavy bleeding like a very heavy period. Bright red at first, gradually turning pink then brown. Normal for 2-6 weeks.
- Uterus shrinking: Your uterus went from fist-sized to watermelon-sized during pregnancy. Now it's contracting back down. You'll feel cramping, especially while breastfeeding (oxytocin causes contractions).
- Perineal pain: If you tore or had an episiotomy, you're healing. Sitting hurts. Going to the bathroom is terrifying. Use a peri bottle, ice packs, and witch hazel pads.
- C-section incision healing: If you had a C-section, your incision needs 6-8 weeks to heal internally. Moving, lifting, and even coughing can hurt.
- Breast engorgement: Milk comes in around day 2-5. Your breasts might feel rock-hard and painful until supply regulates.
- Night sweats: Drenching sweats as your body sheds pregnancy fluid and adjusts hormones.
- Extreme fatigue: You're not sleeping more than 2-3 hours at a time. Your body is healing. This is survival mode.
What helps:
- Take pain medication as prescribed—don't try to tough it out
- Rest whenever the baby sleeps (ignore the housework)
- Accept help—let others cook, clean, hold the baby while you shower
- Stay hydrated (especially if breastfeeding)
- Use cooling pads, sitz baths, stool softeners
Weeks 3-6: Still Healing, Slightly Less Awful
What's happening:
- Bleeding slows: Lochia should be lighter now—pink or brown discharge. If it suddenly turns bright red again, call your doctor.
- Uterus almost back to normal: By 6 weeks postpartum, your uterus is nearly back to pre-pregnancy size.
- Perineal healing: Most tearing or episiotomies heal by week 4-6, but you might still feel tenderness.
- Energy slightly improving: You're still exhausted, but maybe you can walk around the block without feeling wrecked.
- Emotions stabilizing: If you had baby blues, they usually lift by week 3. If they don't, it might be postpartum depression (more below).
What helps:
- Gentle movement—short walks, light stretching (NOT intense workouts yet)
- Postpartum checkup (ACOG recommends initial contact within 3 weeks and a comprehensive visit by 12 weeks[7]), don't skip it
- Start pelvic floor exercises if your doctor clears you
Weeks 7-12: The "New Normal" Emerges
What's happening:
- Bleeding stops: By 6-8 weeks, lochia should be done. If not, see your doctor.
- Physical healing mostly complete: Incisions healed, perineum recovered, uterus back to size.
- Hormones stabilizing: Still not back to pre-pregnancy levels, but no longer in freefall.
- Sleep slightly better: Some babies start sleeping in longer stretches (but not all—don't compare yourself to Instagram moms).
- Hair loss starts: Around month 3-4, you might notice clumps of hair falling out. This is normal—your hair stopped shedding during pregnancy, now it's catching up.
What helps:
- Gradual return to exercise (if cleared by your doctor)
- Pelvic floor physical therapy if you're having pain, leaking, or prolapse symptoms
- Finding your new routine (it won't look like your old one)
Baby Blues vs. Postpartum Depression: How to Tell the Difference
Research suggests that up to 76% of new mothers experience "baby blues" in the first 2 weeks, though pooled estimates put the average closer to 40%.[3] This is different from postpartum depression (PPD), which affects roughly 14% of new mothers and requires treatment.[4]
Baby Blues (Normal, Temporary)
Symptoms:
- Crying for no clear reason
- Mood swings—happy one minute, overwhelmed the next
- Anxiety about the baby
- Feeling exhausted and overwhelmed
- Trouble sleeping even when the baby sleeps
Timeline: Starts around day 2-3 after birth, peaks around day 5-7, resolves by week 2-3
Why it happens: The hormone crash, sleep deprivation, and life adjustment
What helps: Rest, support, talking about how you feel, time
Postpartum Depression (Needs Treatment)
Symptoms:
- Persistent sadness, hopelessness, or emptiness that doesn't lift
- Loss of interest in things you used to enjoy
- Difficulty bonding with the baby
- Feeling like you're failing as a mother
- Withdrawing from family and friends
- Severe anxiety or panic attacks
- Intrusive scary thoughts about the baby or yourself
- Inability to sleep even when exhausted, or sleeping too much
- Thoughts of harming yourself or the baby
Timeline: Can start anytime in the first year, but most common in the first 3 months[4]
Why it happens: Hormonal changes, sleep deprivation, history of depression, lack of support, birth trauma
What helps: Therapy, medication (safe for breastfeeding), support groups, asking for help
This is not your fault. This is not a personal failure.
Postpartum depression is a medical condition caused by hormonal changes, not by being "weak" or "not cut out for motherhood."
If symptoms last longer than 2 weeks or you have thoughts of harming yourself or your baby, call your doctor immediately. PPD is treatable, and you deserve help.
Postpartum Anxiety (Also Common)
Postpartum anxiety affects an estimated 15% of new mothers and can occur alongside or instead of depression.[5]
Symptoms:
- Constant worry about the baby's health or safety
- Racing thoughts that won't stop
- Physical symptoms: racing heart, trouble breathing, dizziness
- Inability to relax or sleep due to worry
- Intrusive thoughts (scary "what if" scenarios)
Postpartum anxiety is also treatable with therapy and medication. Tell your doctor.
When Does Your Period Return?
This is one of the most common postpartum questions—and the answer depends on whether you're breastfeeding.
If You're Not Breastfeeding
Your period typically returns 6 to 13 weeks after birth.[6] Most people get their first postpartum period around 8 to 10 weeks.
What to expect:
- Your first period might be heavier or lighter than normal
- It might be irregular for the first few cycles
- Ovulation can happen 2-4 weeks before your first period, so you CAN get pregnant before your period returns
If You're Breastfeeding
Breastfeeding delays ovulation and menstruation due to elevated prolactin levels. But timing varies widely:
Exclusively breastfeeding (no formula, no long gaps between feeds):
- Period might not return for 6+ months, sometimes up to 12+ months
- The more frequently you nurse, the longer menstruation is suppressed
- Night nursing is especially important for delaying ovulation
Combination feeding (breast + formula):
- Period returns sooner, often within 3-6 months
- Less breastfeeding = faster return of ovulation
When baby starts solids or sleeping through the night:
- Nursing frequency drops, prolactin levels drop, ovulation returns
- Many people get their first period around 6-9 months postpartum when this happens
- Once your cycle returns, you can start syncing your lifestyle to your cycle phases to optimize energy, workouts, and nutrition
Important: You can ovulate BEFORE your first postpartum period. If you don't want to get pregnant right away, use birth control even if you haven't had a period yet. "Breastfeeding as birth control" only works under very specific conditions (exclusive breastfeeding, baby under 6 months, no period return)—and even then it's only about 98% effective.
What About Pelvic Floor Recovery?
Pregnancy and birth put a lot of stress on your pelvic floor—the muscles that support your bladder, uterus, and bowels. Recovery is important, but it takes time.
Common Postpartum Pelvic Floor Issues
- Urinary leaking: When you cough, sneeze, laugh, or jump
- Painful sex: Vaginal dryness (especially if breastfeeding), scar tissue, muscle tension
- Pelvic pressure or heaviness: Possible pelvic organ prolapse
- Back or hip pain: Pelvic floor dysfunction can cause referred pain
- Bowel issues: Constipation or trouble controlling bowel movements
What helps:
- Pelvic floor physical therapy (not just Kegels—see a specialist)
- Gradual return to exercise (avoid high-impact too soon)
- Core and pelvic floor coordination (not just strengthening)
- Address diastasis recti if present (abdominal separation)
Don't accept "this is just part of being a mom." Leaking and pain are common, but they're treatable. See a pelvic floor PT if you're having any of these issues.
When to Call Your Doctor
Some symptoms need immediate attention. Call your doctor or go to the ER if you experience:
Emergency Symptoms
- Heavy bleeding: Soaking through a pad in less than an hour, passing clots larger than a golf ball
- Fever over 100.4°F: Could indicate infection
- Severe abdominal pain: Especially if accompanied by fever
- Chest pain or trouble breathing: Could be a blood clot (postpartum is a high-risk time for clots)
- Severe headache with vision changes: Possible postpartum preeclampsia
- Red, swollen, hot, painful breast: Possible mastitis (breast infection)
- Foul-smelling vaginal discharge: Could indicate infection
- Thoughts of harming yourself or your baby: Call your doctor or 988 (Suicide & Crisis Lifeline) immediately
Non-Emergency But Still Call
- Bleeding that suddenly gets heavy after improving
- Incision that's red, swollen, oozing, or separating
- Symptoms of depression or anxiety lasting longer than 2 weeks
- Pain that's getting worse instead of better
- Urinary leaking that's not improving after 6-8 weeks
Tracking Your Postpartum Recovery
The fourth trimester is overwhelming. You're managing a newborn, recovering physically, and dealing with massive hormonal shifts. Tracking your symptoms can help you:
- Know what's normal for YOU vs. when something's off
- Identify patterns (like when bleeding increases after too much activity)
- Communicate clearly with your doctor at checkups
- Track mood changes to catch postpartum depression early — learn more about why mood tracking matters for women's health
- See your progress—recovery isn't linear, but tracking shows you're healing
What to track:
- Bleeding (color, amount, clots)
- Pain levels (incision, perineal, cramping)
- Mood and energy levels
- Sleep (when and how much)
- Breastfeeding (if applicable)
- Physical symptoms (night sweats, headaches, breast changes)
- Return of period or ovulation signs
Go Go Gaia helps with postpartum tracking:
- Switch to "Postpartum Mode" to track recovery-specific symptoms
- Log bleeding, pain, mood, and sleep in one place
- Track baby's feeding schedule alongside your recovery
- Get reminders for postpartum checkups
- Export your data to share with your doctor
- Track when your period returns after pregnancy
Track your postpartum recovery and know what's normal
The Bottom Line
The fourth trimester is hard. Harder than most people admit.
Your hormones crashed. Your body is healing from something massive. You're not sleeping. You're learning to care for a newborn. And everyone expects you to be glowing and grateful.
You can be grateful and struggling at the same time. You can love your baby and miss your old life. You can be healing and also need help.
What's normal:
- Bleeding for 4-6 weeks
- Feeling exhausted
- Night sweats
- Mood swings in the first 2 weeks
- Soreness and pain while healing
- Not feeling "back to normal" for months
What's not normal (and needs a doctor):
- Heavy bleeding that soaks through a pad in an hour
- Fever, severe pain, or foul-smelling discharge
- Depression or anxiety that lasts longer than 2 weeks
- Thoughts of harming yourself or your baby
- Physical symptoms getting worse instead of better
Recovery takes 6-12 weeks physically. Emotionally and hormonally? Longer. And that's okay.
Ask for help. Track your symptoms. Trust your gut when something feels wrong. And give yourself more grace than you think you need.
You just did something incredible. Your body needs time to recover.
Related Reading
Complete Guide to Pregnancy Tracking
Learn what to track during pregnancy to prepare for postpartum recovery.
Wellness Tips for Each Trimester
Essential health tracking and wellness practices for every stage of pregnancy.
Am I Pregnant? Early Signs and When to Test
Learn the early signs of pregnancy and when to take a test for accurate results.
Complete Guide to Period Tracking
Learn what to track and how to use your cycle data after your period returns.
References
This guide is based on current medical evidence and clinical guidelines. Key sources include:
- Dukic J, Johann A, Henninger M, Ehlert U. Estradiol and progesterone from pregnancy to postpartum: a longitudinal latent class analysis. Front Glob Womens Health. 2024;5:1428494. doi:10.3389/fgwh.2024.1428494.
- Trifu S, Vladuti A, Popescu A. The neuroendocrinological aspects of pregnancy and postpartum depression. Acta Endocrinologica (Bucharest). 2019;15(3):410–415. doi:10.4183/aeb.2019.410. PMID: 32010366.
- Rezaie-Keikhaie K, Arbabshastan ME, Rafiemanesh H, et al. Systematic review and meta-analysis of the prevalence of the maternity blues in the postpartum period. J Obstet Gynecol Neonatal Nurs. 2020;49(2):127–136. doi:10.1016/j.jogn.2020.01.001. PMID: 32035973.
- Liu X, Wang S, Wang G. Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J Clin Nurs. 2022;31(19-20):2665–2677. doi:10.1111/jocn.16121. PMID: 34750904.
- Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. 2017;210(5):315–323. doi:10.1192/bjp.bp.116.187179. PMID: 28302701.
- Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactating women: a systematic review. Obstet Gynecol. 2011;117(3):657–662. doi:10.1097/AOG.0b013e31820ce18c. PMID: 21343770.
- ACOG Committee Opinion No. 736: Optimizing Postpartum Care. Obstet Gynecol. 2018;131(5):e140–e150. doi:10.1097/AOG.0000000000002633. PMID: 29683911.
For personalized medical advice about postpartum recovery, always consult with qualified healthcare professionals.