Pregnancy Tracking Guide 2026: What to Track Each Trimester

From first symptoms to counting kicks, learn what to track during pregnancy for a more confident, empowered experience—backed by science and designed to reduce overwhelm.
Important Medical Disclaimer
This article is for educational and informational purposes only and does not constitute medical advice or prenatal care. Every pregnancy is unique, and the information provided should not replace consultation with your healthcare provider. Always consult your OB-GYN, midwife, or healthcare provider before making any changes to your pregnancy care routine, and follow their personalized recommendations for your specific situation.
If you experience any concerning symptoms, warning signs, or have questions about your pregnancy, contact your healthcare provider immediately. When in doubt, always call your doctor—they would rather hear from you than have you wait. Your prenatal care team is your best resource for guidance throughout your pregnancy.
Sarah stared at her phone at 2 AM, searching "is it normal to feel..." for the third time that night. As a first-time mom at 12 weeks pregnant, she was overwhelmed by contradictory advice, worried about every twinge, and couldn't remember if she'd felt this nauseous last week or if it was getting worse. Her next prenatal appointment was two weeks away, and she wasn't sure what was worth mentioning to her doctor.
Sound familiar? You're not alone. Many pregnant women navigate a confusing landscape of physical changes, emotional shifts, and information overload—all while trying to figure out what's "normal" and what needs medical attention. (If you're still in the "is this happening?" phase, check out our guide on early pregnancy signs and when to test.)
This is where pregnancy tracking becomes your superpower. Not the obsessive, anxiety-inducing kind of tracking—but thoughtful, pattern-based monitoring that helps you understand your unique pregnancy, communicate effectively with your healthcare provider, and feel more confident.
Why Pregnancy Tracking Matters: The Science
Before diving into what to track, let's talk about why it matters. Research suggests that women who actively monitor their pregnancy health report feeling more prepared for prenatal appointments and more confident in recognizing potential concerns. Here's what tracking can offer:
- Better communication with your healthcare provider: Concrete data helps your doctor understand your experience beyond a single appointment snapshot
- Early pattern recognition: Tracking helps you notice gradual changes that might otherwise go unnoticed
- Reduced anxiety: When you can see patterns (like "nausea is always worse when I sleep poorly"), symptoms feel less random and frightening
- Personalized insights: Every pregnancy is different—tracking helps you understand YOUR pregnancy, not just generic symptoms
- Preparation for appointments: Never forget important questions or symptoms to mention
- Memory preservation: Pregnancy brain is real! Tracking captures details you'd otherwise forget
Important Note
Tracking should empower you, not increase anxiety. If you find that tracking every symptom makes you more worried, focus only on key metrics your healthcare provider recommends. The goal is confidence, not stress.
Understanding Pregnancy Changes: What's Happening in Your Body
Pregnancy triggers dramatic hormonal and physical changes. Understanding the science helps you know what to expect and why tracking matters.
The Hormone Cascade
Four main hormones orchestrate pregnancy:
- HCG (Human Chorionic Gonadotropin): Rises rapidly in early pregnancy, doubling approximately every 48 hours in early weeks.[1] This is what pregnancy tests detect and what often causes first-trimester nausea.[2]
- Progesterone: Increases throughout pregnancy to maintain the uterine lining and prevent contractions. Side effects may include fatigue, constipation, and mood changes.
- Estrogen: Rises steadily to support fetal development and prepare your body for birth. Can affect mood, skin, and circulation.
- Relaxin: Helps ligaments soften to prepare for birth, which can cause joint discomfort and changes in posture.
These hormones don't just affect your uterus—they influence your entire body, from your digestive system to your brain chemistry. This is why pregnancy symptoms are so varied and why your experience will be unique.
Here's how these three key hormones change from conception through birth:
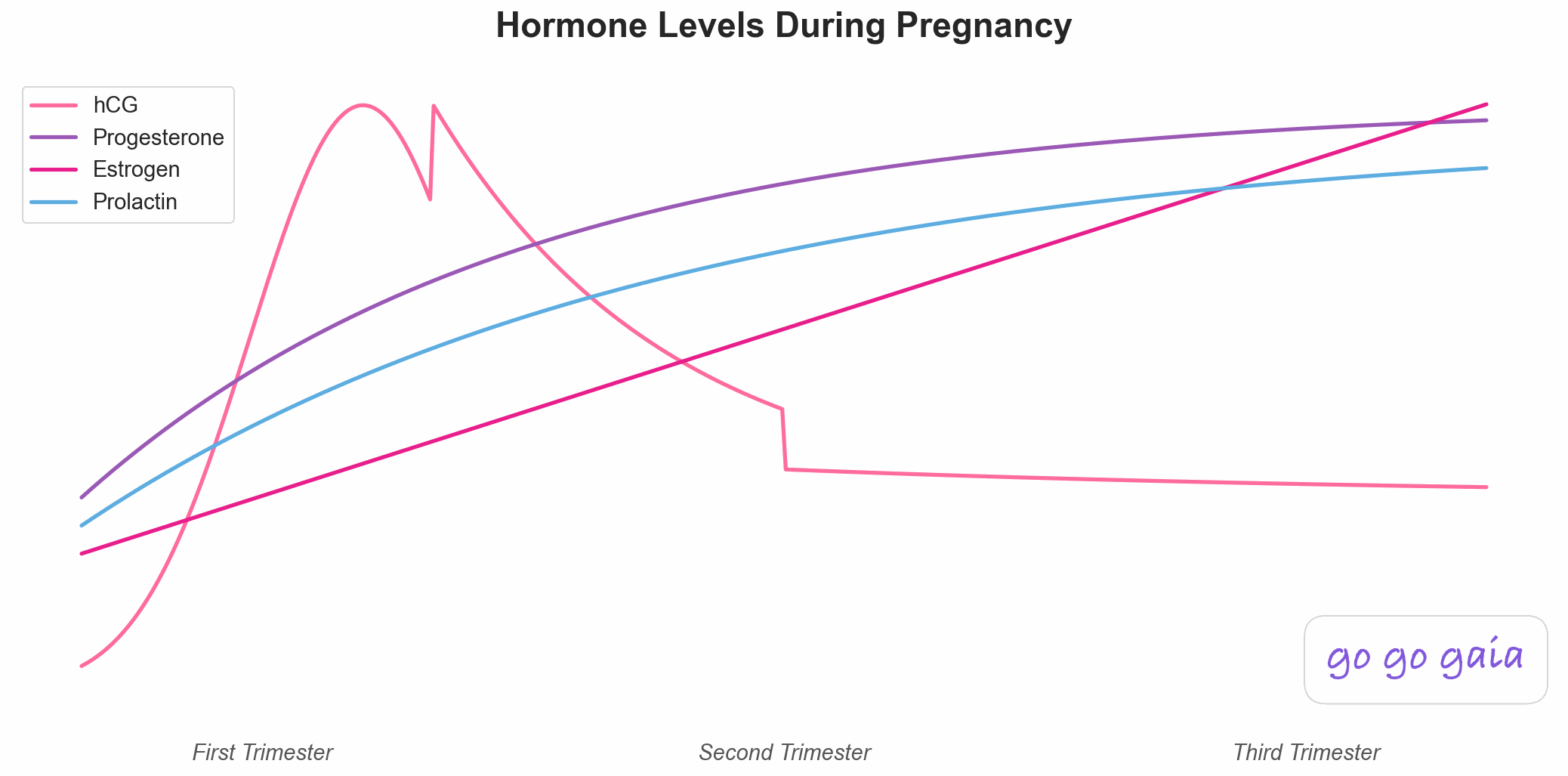
Hormone changes throughout all three trimesters of pregnancy
Notice the dramatic HCG spike in the first trimester that peaks around weeks 8-11—this timing directly corresponds to when morning sickness is typically most severe. As HCG declines in the second trimester, most women feel significant relief from nausea. Meanwhile, progesterone and estrogen continue rising steadily throughout pregnancy, supporting your growing baby and preparing your body for birth.
Trimester-by-Trimester Tracking Guide
What you track—and how intensively—will change as your pregnancy progresses. Here's your comprehensive guide for each stage.
First Trimester (Weeks 1-13): The Foundation Phase 🌱
What's Happening
From conception through the first 13 weeks, your baby transforms from a fertilized egg to a fully formed fetus with all major organs developing. Your body is working incredibly hard even though you may not look pregnant yet. HCG levels peak around weeks 10-11, which is often when nausea is most intense.
This zoomed-in view of first trimester hormones shows the dramatic early changes:

Hormone changes during the first trimester (Weeks 1-13)
The exponential HCG curve you see here is what makes early pregnancy confirmation possible—HCG doubles every 48-72 hours in a healthy early pregnancy, which is why pregnancy tests become more reliable as days pass. The peak around weeks 8-11 isn't coincidental; this is exactly when morning sickness tends to be worst. Understanding this pattern helps you know that the nausea, while miserable, is actually a sign of a healthy, progressing pregnancy.
Common Experiences
Many women experience fatigue, nausea or "morning sickness" (which can occur any time of day—affecting up to 70% of pregnant women)[2], breast tenderness, frequent urination, food aversions or cravings, heightened sense of smell, mood swings, and bloating. Some women have minimal symptoms, which is also completely normal.
What to Track
- Nausea and vomiting: Time of day, severity, triggers, what helps
- Fatigue levels: Note extreme exhaustion that interferes with daily life
- Bleeding or spotting: Amount, color, when it occurs (some light spotting can be normal, but always mention to your provider)
- Food aversions and cravings: Helps identify patterns and ensure adequate nutrition
- Prenatal vitamin intake: Consistency matters, especially for folic acid
- First prenatal appointments: Questions to ask, test results received
- Mood and anxiety levels: Prenatal mood changes are common but worth monitoring
Red Flags to Track and Report Immediately
Call your healthcare provider immediately if you experience:
- Heavy vaginal bleeding (soaking through a pad in an hour)
- Severe, sharp abdominal or pelvic pain
- Severe nausea/vomiting that prevents keeping any food or liquids down
- Fever over 100.4°F (38°C)
- Painful urination or signs of infection
- Sudden complete disappearance of all pregnancy symptoms before 12 weeks
Sample First Trimester Tracking Day
Week 9, Thursday
7:00 AM: Woke up feeling nauseous (7/10), ate crackers before getting up
8:00 AM: Took prenatal vitamin with breakfast (oatmeal - one of few foods that sounds good)
10:00 AM: Nausea improved to 4/10 after eating
12:00 PM: Light lunch (chicken soup), still feeling okay
2:00 PM: Fatigue hitting hard—needed to rest
6:00 PM: Nausea returning (6/10), smell of cooking meat triggering it
9:00 PM: Early bedtime—exhausted
Notes: Definitely noticing pattern—nausea worse in morning and evening. Chicken and bland foods helping. Ask doctor about safe anti-nausea options at next appointment.
Second Trimester (Weeks 14-27): The Energy Return Phase 🌸
What's Happening
Often called the "golden period" of pregnancy, many women experience renewed energy as HCG levels stabilize and nausea subsides (typically resolving by 16-20 weeks).[2] Your baby is growing rapidly, and you'll likely start showing. The most exciting milestone: feeling your baby move for the first time (quickening), typically between 16-25 weeks.
Common Experiences
Reduced nausea and increased energy for many women, visible baby bump, first movements ("flutters" then stronger kicks), round ligament pain (sharp pains in lower abdomen with movement), backaches as your center of gravity shifts, skin changes (darkening, linea nigra, possible melasma), and increased appetite. Some women may experience Braxton Hicks contractions starting in this trimester.
What to Track
- First movements: Date you first feel movement, patterns as they develop
- Movement patterns: Once you feel regular movements, note times of day baby is most active
- Weight changes: Your healthcare provider will monitor this, but tracking trends between appointments can be helpful
- Physical discomforts: Back pain, round ligament pain, headaches—note severity and frequency
- Sleep quality: As your belly grows, sleep may become more challenging
- Swelling: Mild swelling in feet and ankles is common, but sudden severe swelling needs attention
- Glucose screening results: Usually done between 24-28 weeks
- Anatomy scan findings: Typically performed around 18-22 weeks
Red Flags to Track and Report Immediately
Call your healthcare provider immediately if you experience:
- Absence of movement after you've started feeling regular movements
- Sudden, severe swelling (especially face and hands)
- Severe, persistent headache that doesn't respond to usual remedies
- Vision changes (blurriness, seeing spots, temporary vision loss)
- Severe abdominal pain
- Signs of preterm labor: regular contractions, pelvic pressure, fluid leaking
- Vaginal bleeding
Sample Second Trimester Tracking Day
Week 24, Monday
7:30 AM: Slept pretty well (side sleeping with pillow between knees helping)
9:00 AM: First baby movements today—little flutters while sitting at desk
12:00 PM: Appetite is BACK—ate a full lunch plus snack
3:00 PM: Sharp pain in right side when I stood up too fast (round ligament pain—mentioned to doctor last visit, she said normal)
7:00 PM: Baby very active during dinner—lots of kicks and rolls
9:00 PM: Mild lower back ache—pregnancy pillow and heating pad helping
Notes: Noticing baby is most active in the evening. No swelling today. Feeling generally great—so much better than first trimester!
Third Trimester (Weeks 28-40+): The Home Stretch Phase 🍂
What's Happening
Your baby is gaining weight rapidly and positioning for birth. You're getting close to meeting your little one! Your body is preparing for labor with practice contractions (Braxton Hicks), and you may experience a burst of energy called "nesting" in the final weeks.
Common Experiences
Fatigue returning, frequent urination (baby pressing on bladder), shortness of breath (uterus pressing on diaphragm), Braxton Hicks contractions (irregular, painless tightening), backaches and pelvic pressure, heartburn and indigestion, difficulty sleeping, swelling in feet and ankles, and increased baby movements (though they may feel different as space gets tighter).
What to Track
- Kick counts: Starting around 28 weeks, your healthcare provider may recommend monitoring fetal movements daily
- Contractions: Timing, frequency, intensity (distinguish Braxton Hicks from real labor)
- Swelling: Note location and severity, especially sudden changes
- Sleep positions and quality: Important for both comfort and fetal health
- Physical symptoms: Pelvic pressure, lightning crotch, back pain
- Signs of labor: Mucus plug, bloody show, water breaking, regular contractions
- Nesting activities: The sudden urge to prepare everything
- Weight and blood pressure: Monitored closely at appointments
- Questions for delivery planning: Track things you want to discuss with your care team
Red Flags to Track and Report Immediately
Call your healthcare provider immediately if you experience:
- Decreased fetal movement or significant change in movement patterns
- Regular contractions before 37 weeks (every 10 minutes or less)
- Fluid leaking from vagina (potential water breaking)
- Sudden severe swelling, especially with headache or vision changes
- Severe, persistent headache
- Vaginal bleeding
- Severe abdominal pain
- Signs of preeclampsia: severe headache, vision changes, right upper abdominal pain
Understanding Kick Counts
Your healthcare provider will give you specific guidance, but a common recommendation is to track how long it takes to feel 10 movements (kicks, rolls, jabs). Many providers suggest this should happen within 2 hours, though some babies are naturally more active than others. The key is knowing YOUR baby's normal pattern and noticing significant changes.
Sample Third Trimester Tracking Day
Week 36, Friday
6:00 AM: Woke up three times to pee (normal now), some back discomfort
8:00 AM: Baby active after breakfast—counted 10 movements in 45 minutes
11:00 AM: Braxton Hicks contraction—belly got tight for about 30 seconds, no pain
2:00 PM: Feet are swelling—elevating them now
4:00 PM: Sudden burst of energy—organized the entire nursery closet (nesting!)
8:00 PM: Another Braxton Hicks, still irregular
10:00 PM: Baby movements slowing down for the night (this is their normal pattern)
Notes: Swelling is mild and goes down when I rest. Braxton Hicks not increasing in frequency. Packed hospital bag today. Ready to meet this baby!
Key Metrics to Track Throughout Pregnancy
While some things are trimester-specific, these metrics are valuable to monitor throughout your entire pregnancy:
Physical Health
- Weight: Your healthcare provider will track this at appointments and provide personalized guidance based on your pre-pregnancy BMI
- Blood pressure: Checked at every prenatal appointment; tracking helps identify trends
- Symptoms: Headaches, swelling, nausea, pain—note frequency, severity, and triggers
- Exercise and activity: With your provider's approval, tracking movement helps maintain healthy habits
- Hydration: Many women find tracking water intake helpful
Baby's Development
- Movements: After you start feeling them, patterns become important
- Heartbeat: Heard at prenatal appointments (not recommended to use home dopplers without medical guidance)
- Growth measurements: Fundal height, ultrasound measurements
Emotional Wellbeing
- Mood: Prenatal anxiety and depression are common and treatable
- Stress levels: Note triggers and coping strategies
- Sleep quality: Both quantity and quality matter
- Support system: Who you're turning to and whether you need more support
Mental Health Matters
If you're experiencing symptoms of prenatal depression or anxiety—persistent sadness, excessive worry, loss of interest in activities, difficulty bonding with your pregnancy, thoughts of harming yourself—please reach out to your healthcare provider immediately. These conditions are common, treatable, and not your fault.
Crisis resources: If you're having thoughts of self-harm, call 988 (Suicide & Crisis Lifeline) or text "HELLO" to 741741 (Crisis Text Line). Help is available 24/7.
Medical Care
- Appointment dates and findings: What was discussed, test results, next steps
- Medications and supplements: What you're taking (only with provider approval)
- Questions for your provider: Write them down as they occur to you
- Test results: Ultrasounds, glucose screening, Group B strep, etc.
Understanding Your Tracking Patterns: The Real Power
Here's where tracking becomes more than just data collection—it's about discovering correlations and patterns unique to YOUR pregnancy.
Common Patterns to Look For
Sleep and symptoms: Many women notice that poor sleep increases next-day nausea, headaches, or irritability. Identifying this pattern helps you prioritize rest.
Food and nausea: You might notice that eating smaller, more frequent meals reduces nausea, or that certain foods consistently help or hurt.
Hydration and swelling: Counterintuitively, drinking MORE water often helps reduce swelling. Tracking can reveal this pattern.
Activity and discomfort: Understanding which movements trigger round ligament pain or back discomfort helps you adjust activities and know what's normal.
Baby's activity patterns: Most babies develop predictable active and quiet times. Knowing your baby's pattern makes it easier to notice concerning changes.
Real Example
"I tracked my symptoms for three weeks and realized that my afternoon headaches only happened on days I skipped my morning snack. My OB explained that pregnancy can make blood sugar dips worse. Now I keep almonds in my purse, and the headaches are gone!" - Emma, 26 weeks
Preparing for Prenatal Appointments
Your tracked data becomes incredibly valuable at prenatal appointments. Here's how to use it effectively:
Before the Appointment
- Review your tracking notes from the past few weeks
- Write down any concerning symptoms or patterns
- Prepare specific questions (tracked data often prompts good questions)
- Note any symptoms you want to mention, even if they seem minor
During the Appointment
- Share patterns you've noticed (not just isolated symptoms)
- Be specific: "I've had headaches three times this week, all in the afternoon" vs. "I sometimes get headaches"
- Ask for clarification on what's normal vs. what needs monitoring
- Track the provider's advice and recommendations
Questions Your Tracking Might Prompt
- "I've noticed [pattern]—is this normal?"
- "My [symptom] seems to be triggered by [activity/food]—any suggestions?"
- "Should I be concerned that [symptom] has increased/decreased?"
- "Here's my symptom log from the past month—do you see anything concerning?"
When to Call Your Healthcare Provider
Tracking helps you notice trends, but some symptoms need immediate attention regardless of patterns. Trust your instincts—your care team would always rather hear from you than have you wait with a concerning symptom.
Emergency Warning Signs (Any Trimester)
| Symptom | Why It Matters | Action |
|---|---|---|
| Heavy vaginal bleeding | Could indicate miscarriage, placental issues, or other complications | Call immediately or go to ER |
| Severe abdominal pain | Could indicate ectopic pregnancy, placental abruption, or other emergencies | Call immediately or go to ER |
| Decreased fetal movement (after 28 weeks) | Could indicate fetal distress | Call immediately |
| Sudden severe swelling with headache or vision changes | Potential signs of preeclampsia | Call immediately or go to ER |
| Fluid leaking from vagina | Possible water breaking (can happen before labor starts) | Call immediately |
| Fever over 100.4°F | Infection risk to you and baby | Call same day |
| Persistent severe vomiting | Risk of dehydration and nutrient deficiency | Call same day |
| Severe, persistent headache | Could indicate high blood pressure or preeclampsia | Call same day |
| Vision changes (blurriness, spots, flashing lights) | Potential sign of preeclampsia | Call immediately |
| Regular contractions before 37 weeks | Potential preterm labor | Call immediately |
When in Doubt, Call
Trust your instincts. If something feels seriously wrong, don't wait to see if it gets better. Your healthcare provider's office has protocols for urgent situations and can guide you on whether you need to be seen immediately, can wait for an appointment, or can manage symptoms at home. They want to hear from you.
Troubleshooting Common Tracking Challenges
"I Keep Forgetting to Track"
Solution: Set phone reminders, or better yet, use an app with 1-click logging. Go Go Gaia's pregnancy mode makes tracking as simple as tapping a button—no need to remember detailed logs when you're exhausted.
"I'm Overwhelmed by All the Data"
Solution: Start with just 3-5 key metrics your healthcare provider recommends. You don't need to track everything. Focus on what provides value without causing stress.
"I Don't Know What's Normal vs. Concerning"
Solution: This is exactly what tracking helps with! Patterns over time reveal YOUR normal. Bring your tracking log to appointments and ask your provider to help you interpret it.
"Tracking Makes Me More Anxious"
Solution: For some people, tracking increases anxiety rather than reducing it. If this is you, scale back to only what your healthcare provider specifically requests (like kick counts in third trimester). Some women do better with minimal tracking, and that's completely fine.
"I Can't Tell if What I'm Feeling is Braxton Hicks or Real Labor"
Solution: Track the timing, intensity, and pattern. Braxton Hicks are usually irregular, don't increase in intensity, and often stop if you change position or hydrate. Real labor contractions become more regular, intense, and closer together over time. When in doubt, call your provider—they can help you decide if you need to be evaluated.
How Go Go Gaia Makes Pregnancy Tracking Effortless
Let's be honest: pregnancy is exhausting. The last thing you need is a complicated tracking system. Go Go Gaia's pregnancy mode is designed specifically for the realities of pregnancy—quick, intuitive, and actually helpful.
Features Designed for Pregnancy
- Pregnancy mode: Automatically adjusts tracking to pregnancy-relevant metrics
- 1-click symptom logging: Nausea, fatigue, movements—track in seconds, even with pregnancy brain
- Movement tracker: Quick kick counting with patterns over time
- Correlation insights: See connections like "nausea is worse after poor sleep"
- Appointment reminders: Never forget a prenatal visit
- Data export: Share comprehensive tracking logs with your OB-GYN
- Mood tracking: Monitor emotional wellbeing throughout pregnancy
- Customizable: Track what matters to YOU and your specific pregnancy
Real User Story
"I was tracking baby movements on paper and always losing the notes. With Go Go Gaia, I just tap once when baby kicks, and it tracks everything for me. When I mentioned decreased movement to my doctor, I could show her the exact pattern from the past week. Turned out everything was fine, but having that data gave us both confidence." - Rachel, 34 weeks
Pregnancy Tracking Quick Reference
Save this cheat sheet for easy reference throughout your pregnancy:
| Trimester | Key Focus | What to Track | Red Flags |
|---|---|---|---|
| First Weeks 1-13 |
Early development, managing symptoms | Nausea, fatigue, bleeding/spotting, prenatal vitamins, first appointments | Heavy bleeding, severe pain, severe vomiting, fever |
| Second Weeks 14-27 |
Growth, first movements, energy | First kicks, movement patterns, weight, anatomy scan, glucose test, physical discomfort | No movement after it starts, sudden severe swelling, vision changes, severe headache |
| Third Weeks 28-40+ |
Preparation, kick counts, signs of labor | Daily kick counts, contractions, swelling, sleep, signs of labor, nesting | Decreased movement, regular contractions before 37 weeks, fluid leaking, severe swelling + headache |
The Bottom Line
Pregnancy tracking isn't about obsessive monitoring or creating anxiety—it's about empowering yourself with knowledge about YOUR unique pregnancy.
For decades, pregnant women were told to just "listen to their bodies" without tools to understand what their bodies were saying. But now we know better. Thoughtful tracking helps you recognize patterns, communicate effectively with your healthcare provider, and feel more confident navigating the beautiful chaos of pregnancy.
Remember Sarah from the beginning? She started tracking her symptoms and discovered that her nausea followed a predictable pattern—worst in the morning and after poor sleep. She learned which foods helped, recognized that her anxiety spiked on days when she felt isolated, and started reaching out to friends more often. At her 16-week appointment, she could give her doctor a clear picture of her experience, leading to specific recommendations that actually helped.
More importantly, she stopped googling symptoms at 2 AM. She had data, patterns, and confidence.
Your pregnancy is unique. Your tracking should empower you, not stress you out. Start small, focus on what matters, and remember: your healthcare provider is your partner through pregnancy.
You've got this. ❤️
Ready to Track Your Pregnancy with Confidence?
Go Go Gaia's pregnancy mode makes tracking simple with 1-click logging, movement tracking, correlation insights, and data you can share with your OB-GYN.
Try Pregnancy Mode FreeJoin thousands of moms tracking their pregnancy with Go Go Gaia.
Downloadable Resources Coming Soon
We're creating printable trimester tracking checklists and a pregnancy milestone timeline. Check back soon for these free resources!
Frequently Asked Questions
References & Sources
- Larraín D, Caradeux J. β-Human Chorionic Gonadotropin Dynamics in Early Gestational Events: A Practical and Updated Reappraisal. Obstet Gynecol Int. 2024;2024:8351132. doi:10.1155/2024/8351132
- Liu C, Zhao G, Qiao D, Wang L, He Y, Zhao M, Fan Y, Jiang E. Emerging Progress in Nausea and Vomiting of Pregnancy and Hyperemesis Gravidarum: Challenges and Opportunities. Front Med. 2022;8:809270. doi:10.3389/fmed.2021.809270
- Wilcox AJ, Baird DD, Dunson D, McChesney R, Weinberg CR. Natural limits of pregnancy testing in relation to the expected menstrual period. JAMA. 2001;286(14):1759-1761. doi:10.1001/jama.286.14.1759
Note on Sources: This article is informed by peer-reviewed medical research and guidance from leading health organizations including:
- American College of Obstetricians and Gynecologists (ACOG)
- March of Dimes
- National Institutes of Health (NIH)
- Mayo Clinic
- Centers for Disease Control and Prevention (CDC)
Additional peer-reviewed sources on pregnancy tracking outcomes, kick counting recommendations, and other specific pregnancy monitoring topics would strengthen this guide. These represent areas where more published research is needed.