Complete Guide to Menopause: Symptoms, Timeline & What to Expect
You've been through perimenopause. Your periods finally stopped. Now what? Here's what menopause actually is, how it's different from perimenopause, and what changes (or doesn't) after your final period.
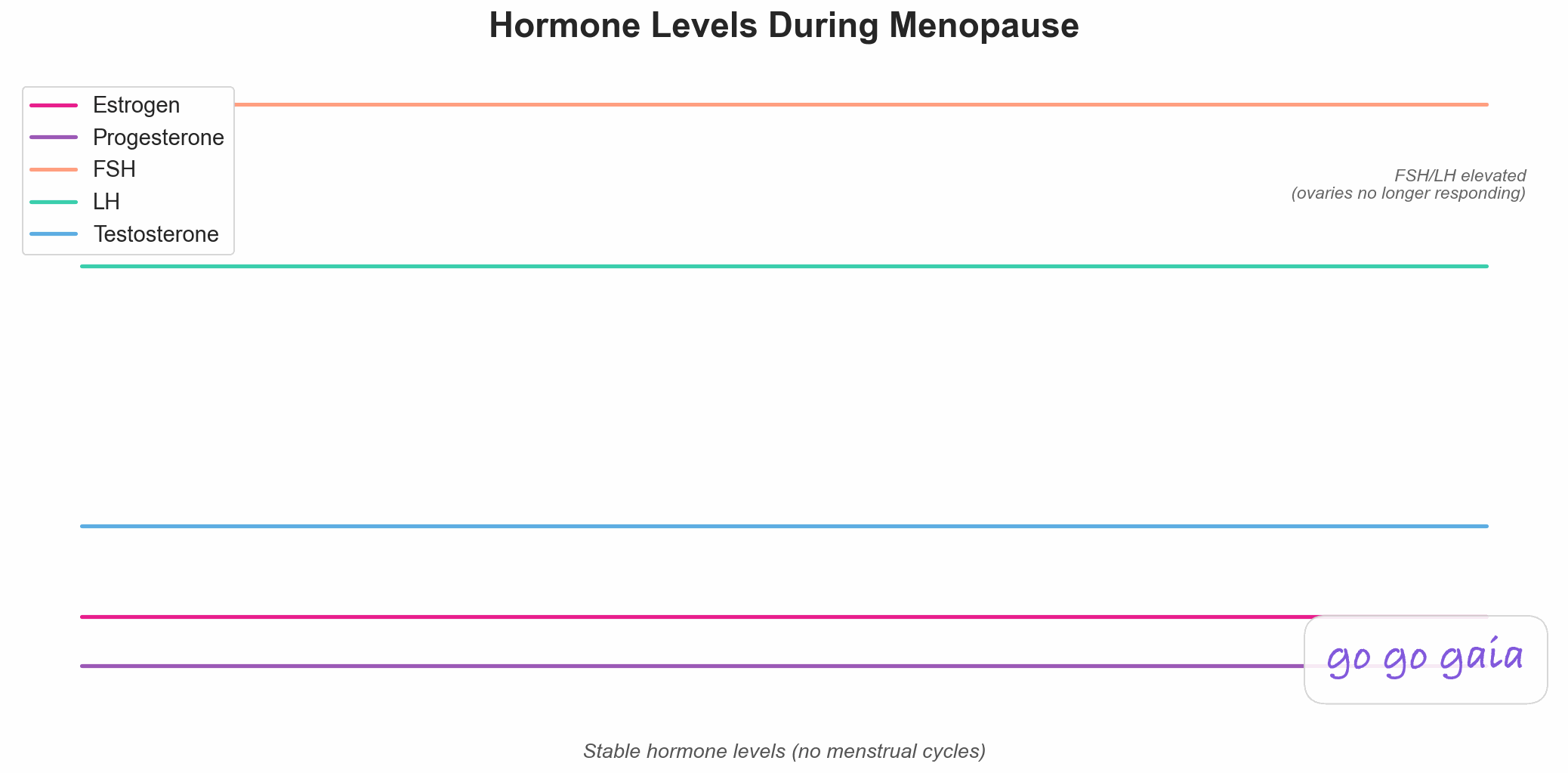
Menopause: stable, flat hormone levels with no more cycles
Medical Disclaimer
This article is for educational and informational purposes only and does not constitute medical advice. The information provided is based on general wellness principles and should not replace consultation with qualified healthcare professionals. Always consult your doctor, gynecologist, or healthcare provider before making significant changes to your diet, exercise routine, or lifestyle, especially if you have underlying health conditions or are considering hormone replacement therapy. If you experience severe symptoms, unexplained bleeding after menopause, or concerns about bone or cardiovascular health, please seek medical attention. Individual results may vary, and what works for one person may not work for another.
Your period didn't come last month. Or the month before. Or for the past year. You're waiting for it to show up again—those erratic perimenopause cycles trained you to expect anything.
But 12 months have passed since your last period. And according to the medical definition, you're now in menopause.
Except nothing feels different. You still have hot flashes. You're still dealing with sleep issues. Your mood hasn't magically stabilized.
So what actually changed? And why does "menopause" feel less like a finish line and more like just... a continuation?
Here's what menopause really is—and what it isn't.
What Is Menopause?
Menopause is defined as 12 consecutive months without a menstrual period. That's it. It's not a phase—it's a single point in time that you can only identify retrospectively.
You don't "enter" menopause. You reach it. Once you hit that 12-month mark, you're considered postmenopausal. Everything after that is postmenopause.
The terminology:
- Perimenopause: The transition years leading up to menopause (typically 4-8 years)
- Menopause: The moment you've gone 12 months without a period
- Postmenopause: All the years after menopause (the rest of your life)
When people say "I'm going through menopause," they usually mean perimenopause. When they say "I'm in menopause," they technically mean postmenopause.
But the distinction matters less than understanding what's happening to your hormones—and why some symptoms persist.
When Does Menopause Happen?
The average age of menopause is 51 years old in the United States, according to data from the Study of Women's Health Across the Nation (SWAN), the largest longitudinal study of the menopausal transition.[1] But "average" doesn't mean much when the range is so wide.
Normal range:
- Most women: 45-55 years old
- Early menopause: 40-45 years old (about 5% of women)
- Premature menopause: Before 40 (about 1% of women)
Factors that influence timing:
- Genetics: You'll likely go through menopause around the same age your mother did
- Smoking: Smokers tend to reach menopause 1-2 years earlier
- Never having been pregnant: May reach menopause slightly earlier
- Chemotherapy/radiation: Can cause early or immediate menopause
- Surgery: Hysterectomy with ovary removal causes immediate menopause
You can't predict exactly when you'll reach menopause, but if your mother went through it at 48, chances are you will too—give or take a few years.
What Happens to Your Hormones
The defining feature of menopause isn't just that your periods stop. It's that your hormones stabilize at new, permanently low levels. No more cycling. No more fluctuations. Just flat, steady hormone levels.
The Hormonal Paradox of Menopause
Menopause creates a hormonal paradox:
- FSH and LH (pituitary hormones): Very high and stable
- Estrogen and progesterone (ovarian hormones): Very low and stable
Your pituitary gland is working overtime, sending out FSH and LH to try to stimulate your ovaries. But your ovaries have run out of viable eggs and no longer respond. So FSH and LH stay elevated while estrogen and progesterone stay low.
This is the opposite of what happens during reproductive years, when FSH surges briefly at the start of each cycle to stimulate egg development, then drops as estrogen rises.
What "Low Estrogen" Means
Estrogen doesn't disappear completely. Your body still produces small amounts from:
- Adrenal glands
- Fat tissue (converts androgens to estrogen)
- Skin, bones, brain
But these sources produce about 10-20% of the estrogen you had during reproductive years. That's enough to keep some functions going but not enough to prevent symptoms or protect against certain health risks.
The Key Difference from Perimenopause
Perimenopause = hormonal chaos. Wild fluctuations. Estrogen spikes and crashes. Some cycles you ovulate, some you don't. Unpredictable symptoms.
Menopause = hormonal stability. Flat, low, predictable hormone levels. No more cycles. No more ovulation. Symptoms may persist, but they're no longer tied to a cycle.
Many women find this stability easier to manage than perimenopause's unpredictability—even if symptoms continue.
Menopause Symptoms: What Changes (and What Doesn't)
Here's the frustrating truth: reaching menopause doesn't automatically make symptoms disappear. Some improve. Some persist. Some are just different.
Symptoms That Often Improve
- Heavy, irregular bleeding: Obviously—you're not menstruating anymore
- PMS: No more cycles means no more premenstrual symptoms
- Hormonal migraines: If yours were tied to estrogen fluctuations, they often improve with stable (low) estrogen
- Mood swings: The emotional volatility of perimenopause often stabilizes in postmenopause. Tracking your mood through this transition helps you see the improvement over time
- Breast tenderness: Usually decreases or disappears
Symptoms That Often Persist or Worsen
- Hot flashes: Can continue for years—average duration is 7-10 years from onset (which was likely in perimenopause)
- Night sweats: Often persist alongside hot flashes
- Vaginal dryness: Worsens over time due to consistently low estrogen (vaginal tissues thin)
- Sleep disruption: May improve slightly but often continues
- Low libido: Can persist or worsen due to low estrogen and testosterone
- Joint pain and stiffness: Common in postmenopause
- Cognitive changes: Brain fog, memory issues may continue
New Concerns in Postmenopause
Low estrogen affects more than just symptoms. It has long-term health implications:
- Bone density loss: Estrogen protects bones. Without it, bone loss accelerates (osteopenia → osteoporosis risk)
- Cardiovascular health: Estrogen protects blood vessels. Risk of heart disease increases after menopause
- Weight redistribution: Fat tends to shift to the abdomen (visceral fat)
- Urinary changes: Increased frequency, urgency, or incontinence
- Skin changes: Thinner, drier skin; more wrinkles (collagen loss)
This isn't aging. This is low estrogen. Some changes would happen with age regardless, but the hormonal shift accelerates certain processes. That's why hormone replacement therapy (HRT) can help—it addresses the root cause.
Perimenopause vs. Menopause: Side by Side
Confused about the difference? Here's a clear comparison:
| Perimenopause | Menopause (Postmenopause) | |
|---|---|---|
| Definition | Transition period before final period | 12+ months since last period |
| Duration | 4-8 years (varies widely) | Rest of your life |
| Periods | Irregular, unpredictable | Absent |
| Hormones | Wildly fluctuating | Stable and low |
| Ovulation | Some cycles yes, some no | No |
| Can you get pregnant? | Yes (until 12 months post-final-period) | No |
| Symptoms | Erratic and cycle-tied | Persistent but predictable |
| What it feels like | Chaotic, unpredictable | Stable but still symptomatic |
If you found perimenopause exhausting because of the unpredictability, postmenopause can feel like relief—even if you still have hot flashes. At least they're consistent.
Managing Menopause Symptoms
You have options beyond "just dealing with it." Treatment depends on symptom severity and personal health factors.
Hormone Replacement Therapy (HRT)
HRT replaces the estrogen (and sometimes progesterone) your body no longer produces. It's the most effective treatment for menopausal symptoms.[2]
What it helps:
- Hot flashes and night sweats (90% reduction for most women)
- Vaginal dryness
- Sleep quality
- Bone density (prevents osteoporosis)
- Possibly mood and cognition
Types of HRT:
- Estrogen-only: For women who've had a hysterectomy
- Estrogen + progesterone: For women who still have a uterus (progesterone protects uterine lining)
- Local estrogen: Vaginal creams/tablets for vaginal symptoms only
When to start: Most effective when started within 10 years of menopause and before age 60. Starting HRT later increases risks.[2]
Risks and benefits: Talk to your doctor. For most healthy women in early postmenopause, benefits outweigh risks.[2] But personal and family history matters (breast cancer, blood clots, heart disease).
Non-Hormonal Options
If HRT isn't right for you:
- SSRIs/SNRIs: Antidepressants can reduce hot flashes by 50-60%
- Gabapentin: Anticonvulsant that helps with hot flashes and sleep
- Vaginal moisturizers and lubricants: For dryness and discomfort
- Lifestyle changes: Layered clothing, fans, avoiding triggers (alcohol, spicy foods, caffeine)
- Cognitive behavioral therapy (CBT): Helps with mood, anxiety, and sleep
Bone Health and Cardiovascular Health
These are long-term priorities in postmenopause:
- Bone density screening: DEXA scan recommended at age 65 (earlier if high risk)
- Weight-bearing exercise: Walking, strength training, resistance exercises—regular physical activity improves bone health, cardiovascular health, mood, and sleep quality.[3] If you use a wearable device, learn how to combine fitness tracking with cycle data for deeper insights
- Calcium and vitamin D: 1,200mg calcium + 800-1,000 IU vitamin D daily
- Heart health: Monitor cholesterol, blood pressure, blood sugar
- Healthy weight: Reduces cardiovascular and bone stress
What About Sex and Relationships?
Low estrogen affects sexual function, but it doesn't mean sex is over. Many women find sex more satisfying in postmenopause once they address the physical changes.
Common issues:
- Vaginal dryness: Makes sex uncomfortable or painful
- Vaginal atrophy: Thinning of vaginal tissues (genitourinary syndrome of menopause)
- Low libido: Less interest in sex due to low estrogen and testosterone
- Difficulty with arousal or orgasm: Changes in blood flow and sensitivity
What helps:
- Vaginal estrogen: Cream, tablet, or ring—highly effective and low-risk
- Lubricants and moisturizers: Non-hormonal options for dryness
- Regular sexual activity: Maintains blood flow and tissue elasticity
- Testosterone therapy: Sometimes prescribed for low libido (off-label)
- Communication: Talk with your partner about what's changed and what you need
Vaginal symptoms don't improve on their own over time—they often worsen. Don't wait to address them.
When to See a Doctor
You should talk to your doctor if:
- You're experiencing symptoms that interfere with daily life or sleep
- You're considering HRT and want to discuss risks and benefits
- You're having vaginal bleeding after 12+ months without a period (needs evaluation—not normal)
- You have severe mood changes, depression, or anxiety
- You're concerned about bone health (family history of osteoporosis, fractures)
- You want to discuss sexual health or vaginal symptoms
You should see a doctor immediately if:
- Heavy bleeding after menopause (soaking through a pad in an hour)
- Any postmenopausal bleeding lasting more than a day
- Severe chest pain or shortness of breath (possible heart issue or blood clot)
- Sudden severe headache or vision changes
Life After Menopause
Menopause isn't the end of anything. It's just a hormonal shift. You're not "old" at 51. You're postmenopausal.
For many women, postmenopause is liberating:
- No more periods, cramps, or PMS
- No more worrying about pregnancy
- No more hormonal chaos (perimenopause was the hard part)
- More emotional stability
- Time to focus on health, career, relationships, hobbies
Yes, there are symptoms. Yes, there are health considerations. But with the right support—medical, lifestyle, social—postmenopause can be a time of clarity and confidence.
Your hormones changed. You didn't.
Track Your Menopause Transition
Go Go Gaia helps you track symptoms, identify patterns, and prepare for doctor appointments—whether you're in perimenopause or postmenopause. Not sure which tracking app is right for you? See our honest comparison of period tracker apps.
With Go Go Gaia, you can:
- Track hot flashes, sleep quality, mood, and other symptoms
- See when symptoms are improving or worsening over time
- Export detailed reports to bring to your doctor
- Log treatments (HRT, supplements) and see what helps
- Get reminders for bone density screenings and health checkups
Track your menopause symptoms and see what helps
References
- Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19(4):387-395. doi:10.1210/jc.2011-3362
- The NAMS 2022 Hormone Therapy Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. doi:10.1097/GME.0000000000002028
- Stojanovska L, Apostolopoulos V, Polman R, Borkoles E. To exercise, or, not to exercise, during menopause and beyond. Maturitas. 2014;77(4):318-323. doi:10.1016/j.maturitas.2014.01.006
Related Reading
Complete Guide to Perimenopause
The transition phase before menopause: symptoms, timeline, and what to expect.
Complete Guide to Cycle Syncing
Learn how to align your workouts, nutrition, and lifestyle with your menstrual cycle.
Understanding PMS: Causes, Symptoms & Relief
Why PMS happens and what actually helps with symptoms.
Complete Guide to Period Tracking
What to track during your cycle and how to use your data to understand your body.