PCOS Guide 2026: Symptoms, Diagnosis & Evidence-Based Management
Polycystic Ovary Syndrome affects 1 in 10 women, yet it takes an average of 2+ years to get diagnosed. Learn everything you need to know about PCOS symptoms, diagnosis, evidence-based treatments, and how tracking helps you take control of your care.
Medical Disclaimer
This article is for educational and informational purposes only and does not constitute medical advice. PCOS is a medical condition that requires diagnosis and management by qualified healthcare professionals. The information provided here is based on current medical evidence but should not replace consultation with your doctor, gynecologist, or endocrinologist. Always seek professional medical advice for diagnosis, treatment options, and personalized care. If you suspect you have PCOS or are experiencing concerning symptoms, please consult a healthcare provider.
Sarah spent years feeling like something was "off." Her periods came every few months, sometimes not at all. She gained weight around her midsection no matter what she tried. Acne along her jawline never cleared up after her teens. Three different doctors told her to "just lose weight" or "it's just stress." At 26, she found a doctor who listened and ran proper tests. The diagnosis? PCOS (Polycystic Ovary Syndrome).
"I was relieved and frustrated at the same time," Sarah says. "Relieved to have an answer. Frustrated it took so long. But once I understood what PCOS was and started tracking my symptoms, everything changed. I wasn't 'broken.' I just needed a different approach."
Sarah's story is incredibly common. PCOS affects approximately 10% of women of reproductive age[6] (that's millions of women), yet diagnosis often takes years. Many women struggle for months or years with irregular periods, unexplained weight gain, fertility challenges, and other symptoms before getting answers.
The good news? PCOS is manageable. With the right information, healthcare team, lifestyle strategies, and tracking tools, you can understand your body, control symptoms, and live a healthy, fulfilling life.
This guide will give you everything you need to know about PCOS: what it is, how it's diagnosed, evidence-based management strategies, and why tracking is one of your most powerful tools.
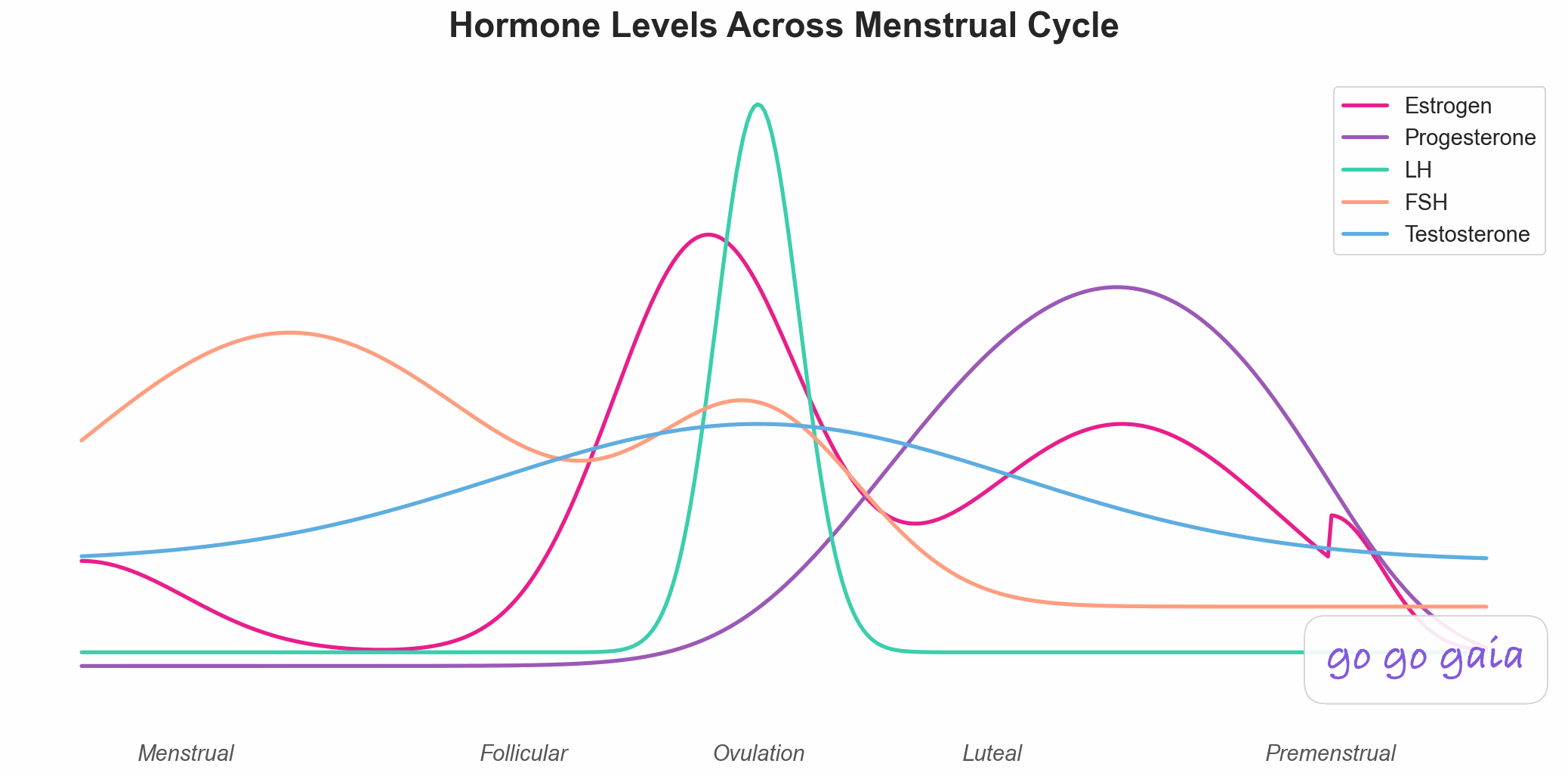
Understanding normal hormone patterns helps identify PCOS disruptions
What is PCOS? Understanding the Basics
The Medical Definition
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder affecting women of reproductive age. It's one of the most common endocrine disorders in women, yet it remains widely misunderstood and underdiagnosed.
Despite the name, you don't need to have ovarian cysts to have PCOS. The term is actually misleading. Many women with PCOS don't have cysts, and many women with ovarian cysts don't have PCOS.
What's Actually Happening in Your Body
PCOS involves several interconnected hormonal imbalances:
1. Elevated Androgens (Hyperandrogenism)
Your body produces higher-than-normal levels of androgens (hormones typically thought of as "male hormones" like testosterone). All women produce some androgens, but with PCOS, levels are elevated. This causes symptoms like excess facial and body hair, acne, and male-pattern hair loss.
2. Insulin Resistance
Up to 70% of women with PCOS have insulin resistance,[6] meaning their cells don't respond normally to insulin. To compensate, the pancreas produces more insulin. High insulin levels trigger the ovaries to produce even more androgens, creating a vicious cycle. Insulin resistance also makes weight loss difficult and increases diabetes risk.
3. Irregular or Absent Ovulation
In a typical menstrual cycle, ovaries develop follicles, one releases an egg (ovulation), and if not fertilized, you get your period about 14 days later. With PCOS, follicles may develop but fail to release an egg. This leads to irregular, absent, or unpredictable periods.
4. Disrupted Hormone Balance
PCOS disrupts the normal balance of estrogen, progesterone, LH (luteinizing hormone), and FSH (follicle-stimulating hormone). Women with PCOS often have elevated LH compared to FSH, which contributes to irregular cycles.
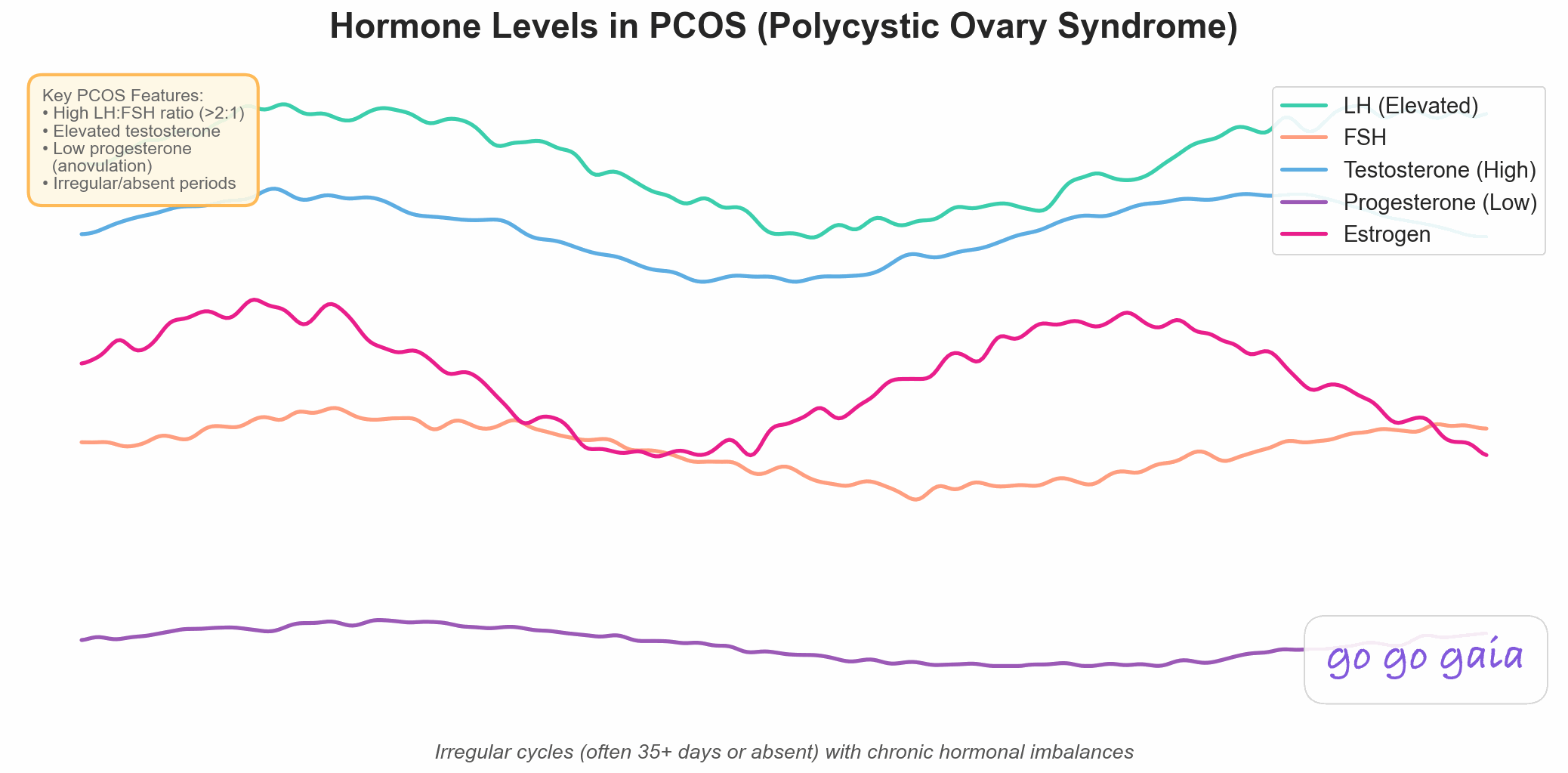
Hormone patterns in PCOS showing elevated LH, high testosterone, and flat progesterone due to anovulation
The Cycle Connection
If you've read our Complete Guide to Cycle Syncing, you know that a typical menstrual cycle has four predictable phases driven by hormonal changes. PCOS disrupts this natural rhythm:
- The follicular phase may be extended as follicles develop slowly or incompletely
- Ovulation may not occur at all (anovulation)
- Without ovulation, there's no true luteal phase
- Periods may be irregular, very light, very heavy, or absent
- Cycle lengths can vary dramatically month to month
Important Clarification
PCOS is a syndrome (a collection of symptoms and signs), not a single disease with one cause. This means PCOS looks different for everyone. Two women with PCOS may have completely different symptoms and experiences. There's no "typical" PCOS presentation, which is why understanding YOUR specific pattern through tracking is so valuable.
PCOS Symptoms: The Complete List
PCOS symptoms vary widely between individuals. Some women have many symptoms; others have only a few. Severity also differs. Here's the complete list of what PCOS can cause:
Menstrual Irregularities
- Irregular periods: Cycles longer than 35 days, or significant variation in cycle length
- Absent periods (amenorrhea): Fewer than 8 periods per year, or no period for several months
- Unpredictable cycles: Never knowing when your period will arrive
- Very light or very heavy bleeding: Flow intensity that varies significantly
- Prolonged bleeding: Periods lasting longer than 7 days
Hyperandrogenism (High Androgen Symptoms)
- Hirsutism (excess hair): Affects about 70% of women with PCOS.[6] Dark, coarse hair growing on the face (upper lip, chin, sideburns), chest, back, abdomen, or inner thighs
- Acne: Especially along the jawline, chin, and lower face. Often resistant to typical acne treatments
- Oily skin: Excess sebum production
- Male-pattern hair loss: Thinning hair on the scalp, especially at the crown and temples
Metabolic Symptoms
- Weight gain: Especially around the midsection (abdominal or visceral fat)
- Difficulty losing weight: Even with diet and exercise, weight loss is challenging
- Insulin resistance: Affects 50-70% of women with PCOS
- Dark skin patches (acanthosis nigricans): Velvety, dark patches of skin in body folds like the neck, armpits, groin, or under breasts (a sign of insulin resistance)
- Increased hunger and cravings: Especially for carbohydrates and sugars
- Fatigue: Persistent low energy, especially after meals
Fertility and Reproductive Health
- Difficulty getting pregnant: PCOS is one of the leading causes of female infertility due to irregular or absent ovulation
- Increased miscarriage risk: Higher rates in the first trimester
- Pregnancy complications: Higher risk of gestational diabetes, preeclampsia, and preterm birth
Other Common Symptoms
- Mood changes: Increased rates of anxiety and depression
- Sleep issues: Difficulty sleeping, increased risk of sleep apnea
- Skin tags: Small skin growths, often on the neck or armpits
- Pelvic pain: Some women experience pain (though not universal)
The Tracking Insight
Every woman's PCOS looks different. Tracking YOUR specific symptoms helps you understand YOUR pattern and identify what works for YOUR body, not just generic PCOS advice. After tracking for 2-3 months, patterns emerge that guide personalized management strategies.

Consistent tracking helps identify your unique PCOS patterns and what interventions work for you
How is PCOS Diagnosed?
Getting a PCOS diagnosis often takes time and persistence. Many women see multiple doctors before receiving proper testing and diagnosis. Here's what the diagnostic process involves:
The Rotterdam Criteria
PCOS is diagnosed using the Rotterdam criteria,[1] established by the European Society of Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM). You need 2 out of the following 3 criteria:
Rotterdam Criteria (Need 2 of 3)
- Irregular ovulation or anovulation - Shown by irregular periods, absent periods, or lack of ovulation confirmed through testing
- Clinical or biochemical signs of hyperandrogenism - Either blood tests showing elevated androgens OR physical signs like hirsutism, acne, or hair loss
- Polycystic ovaries on ultrasound - 12 or more follicles (2-9mm) per ovary, or ovarian volume greater than 10cm³
Other conditions that cause similar symptoms must be ruled out, including thyroid disorders, hyperprolactinemia, and congenital adrenal hyperplasia.
The Diagnostic Process
1. Medical History and Symptom Review
Your doctor will ask about:
- Menstrual cycle history (cycle length, regularity, flow)
- Weight changes and difficulty losing weight
- Excess hair growth, acne, or hair loss
- Fertility challenges or pregnancy history
- Family history of PCOS, diabetes, or metabolic disorders
- Other symptoms (fatigue, mood changes, sleep issues)
This is where tracking becomes invaluable. Bringing 3-6 months of tracked cycle data showing your period dates, cycle lengths, symptoms, and their timing can dramatically speed up diagnosis and help your doctor see clear patterns. Learn what to track in our complete period tracking guide.
2. Physical Examination
Your doctor will check for:
- Signs of excess androgen (hirsutism, acne, male-pattern hair loss)
- Acanthosis nigricans (dark skin patches indicating insulin resistance)
- Body mass index (BMI) and waist circumference
- Blood pressure
3. Blood Tests
Comprehensive blood work typically includes:
- Androgen levels: Total testosterone, free testosterone, DHEA-S
- Reproductive hormones: LH, FSH (often elevated LH:FSH ratio in PCOS), estradiol, progesterone
- Metabolic markers: Fasting glucose, fasting insulin, hemoglobin A1c (diabetes screening), lipid panel
- Thyroid function: TSH, free T4 (to rule out thyroid disorders)
- Prolactin: To rule out hyperprolactinemia
- 17-hydroxyprogesterone: To rule out congenital adrenal hyperplasia
4. Pelvic Ultrasound
A transvaginal or abdominal ultrasound examines your ovaries for:
- Number of follicles (12+ per ovary suggests PCOS)
- Ovarian volume (enlarged ovaries)
- Appearance of ovaries ("string of pearls" pattern of multiple small follicles)
Important note: You can have PCOS without polycystic-appearing ovaries, and you can have polycystic-appearing ovaries without PCOS. The ultrasound is just one piece of the diagnostic puzzle.
Why Tracking Helps with Diagnosis
Bringing tracked data to your doctor appointment can:
- Show clear patterns of irregular cycles (cycle lengths varying by 8+ days)
- Document symptom frequency and severity
- Identify potential ovulation patterns (or lack thereof)
- Provide evidence that prompts doctors to order appropriate tests
- Speed up diagnosis. Instead of "tell me about your periods," you have months of data
- Help rule out other conditions with similar symptoms
Go Go Gaia can generate a detailed health report showing cycle lengths, symptom patterns, and correlations to bring to your doctor appointment. If you're comparing period tracker apps, check out our guide on how to choose the right period tracking app for your needs.
Understanding PCOS Types
Not all PCOS is the same. While the diagnostic criteria are standard, the underlying drivers can differ. Understanding your PCOS "type" helps personalize your management approach:
1. Insulin-Resistant PCOS (Most Common)
Prevalence: Affects 50-70% of women with PCOS[6]
Key features:
- High insulin levels drive excess androgen production
- Weight gain, especially abdominal fat
- Difficulty losing weight despite diet and exercise
- Acanthosis nigricans (dark skin patches)
- Strong carbohydrate cravings
- Energy crashes after meals
Best responds to: Low glycemic index diet, regular exercise, weight loss (even 5-10%), medications like metformin, inositol supplements
2. Inflammatory PCOS
Key features:
- Chronic low-grade inflammation triggers hormonal imbalance
- May be normal weight or lean
- Elevated inflammatory markers (CRP, white blood cells)
- Fatigue, joint pain, headaches
- Skin issues beyond typical PCOS (eczema, psoriasis)
- Food sensitivities or gut issues
Best responds to: Anti-inflammatory diet, stress management, gut health support, omega-3 fatty acids, adequate sleep, reducing environmental toxins
3. Post-Pill PCOS
Key features:
- Symptoms emerge after stopping hormonal birth control
- Periods were regular on the pill but don't return (or are irregular) after stopping
- May be temporary as your body re-establishes natural hormone production
- Can take 6-12 months for cycles to regulate
Best responds to: Patience (allow time for natural cycle to return), cycle tracking to monitor progress, supporting natural hormone production through nutrition and lifestyle, managing androgens naturally
4. Adrenal PCOS
Key features:
- Elevated DHEA-S (an androgen produced by adrenal glands)
- Often related to stress response
- Normal testosterone but high DHEA-S
- May have history of chronic stress or trauma
- Sleep disturbances, anxiety
Best responds to: Stress management, adaptogenic herbs, adequate sleep, nervous system regulation, cortisol management
Why Understanding Your Type Matters
Knowing your PCOS type helps you and your healthcare provider personalize treatment. What works beautifully for insulin-resistant PCOS may not help inflammatory PCOS. Tracking helps you identify which interventions actually improve YOUR symptoms, allowing you to refine your approach over time.
Managing PCOS: Evidence-Based Strategies
PCOS cannot be cured, but it can be effectively managed. For most women, lifestyle changes are the first-line treatment and often the most effective[2] (more powerful than medication alone). Here's what actually works, backed by research:
Nutrition for PCOS
What you eat significantly impacts insulin levels, inflammation, hormone balance, and symptoms. No single diet works for everyone, but these principles are evidence-based:
Blood Sugar Management
Since insulin resistance is central to PCOS for most women, managing blood sugar is crucial:
- Choose low glycemic index (GI) foods: Whole grains instead of refined carbs, legumes, non-starchy vegetables
- Pair carbs with protein and healthy fat: Never eat carbs alone. This prevents blood sugar spikes. Example: apple with almond butter, not apple alone
- Eat frequent, balanced meals: Every 3-4 hours to prevent blood sugar crashes and insulin spikes
- Don't skip breakfast: Eating within 1-2 hours of waking helps regulate blood sugar all day
- Limit refined sugars and processed carbs: White bread, pastries, sugary drinks, candy
Anti-Inflammatory Foods
Reducing inflammation improves insulin sensitivity and hormone balance:
- Omega-3 rich foods: Fatty fish (salmon, sardines, mackerel), walnuts, chia seeds, flaxseeds
- Colorful vegetables: Leafy greens, berries, tomatoes, bell peppers (rich in antioxidants)
- Herbs and spices: Turmeric, ginger, cinnamon (natural anti-inflammatories)
- Healthy fats: Olive oil, avocado, nuts, seeds
- Limit inflammatory foods: Processed foods, trans fats, excessive alcohol, high-sugar foods
Specific Nutrients That May Help PCOS
- Inositol (especially myo-inositol): Improves insulin sensitivity and may restore ovulation. Studies show benefits at 2-4g daily
- Omega-3 fatty acids: Reduces inflammation and androgens. Aim for 2-3 servings of fatty fish per week or supplement
- Magnesium: Improves insulin sensitivity. Found in leafy greens, pumpkin seeds, dark chocolate, almonds
- Vitamin D: Many women with PCOS are deficient. Low vitamin D is associated with insulin resistance. Get levels tested and supplement if needed
- Zinc: May help with acne and hirsutism. Found in oysters, beef, pumpkin seeds
- Chromium: May improve insulin sensitivity. Found in broccoli, whole grains, nuts
Always consult with your doctor or registered dietitian before starting supplements, especially if you're on medications or trying to conceive.
What About Specific Diets?
- Low-carb or ketogenic: Can be effective for some women with insulin-resistant PCOS. May not be sustainable long-term for everyone
- Mediterranean diet: Anti-inflammatory, sustainable, shows benefits for PCOS
- DASH diet: Designed for blood pressure but also helps insulin resistance
- No single "PCOS diet": The best diet is one you can stick with that manages your blood sugar and reduces inflammation
Tracking tip: Use Go Go Gaia to log what you eat and how you feel 1-2 hours later. Over time, you'll see which foods give you energy vs. cause crashes, bloating, or worsened symptoms.
Exercise for PCOS
Exercise is one of the most powerful interventions for PCOS.[5] It improves insulin sensitivity, aids weight management, reduces inflammation, and helps regulate cycles, even without weight loss.
What the Research Shows
- Any exercise is better than none - Even walking helps
- Combination is best: Both cardio and strength training provide benefits
- Aim for 150 minutes per week of moderate activity (or 75 minutes vigorous)
- Strength training 2-3x per week builds muscle, which improves insulin sensitivity
- HIIT can be effective, but don't overdo it. Too much high-intensity exercise can worsen hormonal imbalance
Creating Your PCOS Exercise Plan
- Start where you are: If you're currently sedentary, begin with 10-15 minute walks and build up
- Mix cardio and strength: 3 days cardio + 2 days strength works well for many women
- Include rest days: Recovery is crucial, especially if you have adrenal PCOS
- Find what you enjoy: The best exercise is the one you'll actually do consistently
- Listen to your body: If you're constantly exhausted, you may be overdoing it
Tracking tip: Log your workouts in Go Go Gaia and rate how you felt during and after. You'll discover which types and intensities of exercise improve your energy vs. drain you.
Weight Management
This is a sensitive topic, so let's be clear: Weight gain is a symptom of PCOS, not the cause. You didn't cause your PCOS by gaining weight. The hormonal imbalances of PCOS (especially insulin resistance) make it very difficult to lose weight.
That said, research shows that even 5-10% weight loss can:[2,5]
- Significantly improve insulin sensitivity
- Restore ovulation and regular periods in many women
- Reduce androgen levels (improving acne and hirsutism)
- Improve fertility
- Reduce long-term health risks
Weight loss with PCOS is harder than for women without PCOS. It may take longer and require more consistency. Focus on:
- Sustainable changes, not crash diets
- Non-scale victories: Improved energy, better sleep, clearer skin, more regular cycles
- Health improvements, regardless of weight change
- Self-compassion: You're working against hormonal resistance, not "failing"
Some women with PCOS are lean or normal weight. If that's you, weight loss is NOT your treatment strategy. Focus on the other interventions.
Stress Management
Chronic stress worsens PCOS through multiple mechanisms:
- Elevates cortisol, which increases insulin resistance
- Increases inflammation
- Disrupts reproductive hormones
- Triggers emotional eating and cravings
- Worsens sleep quality
Stress management isn't optional. It's essential:
- Prioritize sleep: Aim for 7-9 hours. Poor sleep worsens insulin resistance
- Practice mindfulness: Meditation, deep breathing, yoga
- Set boundaries: Say no to obligations that drain you
- Therapy or counseling: PCOS is associated with higher rates of anxiety and depression. Professional support helps
- Joyful movement: Exercise that feels good, not punishing
- Social connection: Spending time with supportive people
Tracking tip: Rate your stress level daily in Go Go Gaia. You'll discover when stress spikes and how it correlates with symptom flares, helping you prioritize stress management during vulnerable times.
Medical Treatments for PCOS
Lifestyle changes are foundational, but medication is sometimes necessary and helpful.[2,3] Work with your doctor to determine what's right for you:
Hormonal Birth Control
What it does: Regulates menstrual cycles, reduces androgens, helps with acne and excess hair
Types: Combined oral contraceptive pills, patch, ring (contains estrogen + progestin)
Pros: Reliable period regulation, improves hirsutism and acne, prevents endometrial hyperplasia
Cons: Doesn't treat underlying insulin resistance, side effects vary, not suitable if trying to conceive
Tracking tip: Different formulations affect women differently. Track how you feel on each brand to find the best fit.
Metformin
What it does: Improves insulin sensitivity, lowers insulin and glucose levels
Benefits: May restore ovulation and regular periods, aids weight management, reduces diabetes risk
Pros: Addresses underlying insulin resistance, helps with weight, safe for long-term use
Cons: Gastrointestinal side effects initially (nausea, diarrhea), takes 3-6 months to see full effects
Tracking tip: Monitor how metformin affects your energy, appetite, and GI symptoms. Side effects often improve after the first few weeks.
Anti-Androgen Medications
Spironolactone: Blocks androgen receptors, reduces hirsutism and acne
Timeline: Takes 6-12 months to see full improvement in excess hair
Note: Cannot be used if trying to conceive or pregnant
Tracking tip: Take monthly photos of areas with excess hair to objectively track improvement (it's slow and hard to notice day-to-day).
Fertility Treatments (If Trying to Conceive)
- Letrozole: First-line medication to induce ovulation in PCOS[2]
- Clomid (clomiphene): Also induces ovulation, less effective than letrozole for PCOS
- Metformin: May help restore natural ovulation
- IVF: If other treatments unsuccessful
Tracking tip: Track ovulation signs (cervical mucus, basal body temperature, ovulation tests) to time intercourse and monitor if treatments are working.
PCOS and Your Menstrual Cycle
One of the most frustrating aspects of PCOS is irregular cycles. Understanding how PCOS disrupts your cycle and what to track when cycles are unpredictable helps you take control.
How PCOS Disrupts Normal Cycle Phases
In a typical cycle (as described in our Cycle Syncing Guide):
- Menstrual phase (Days 1-5): Uterine lining sheds
- Follicular phase (Days 6-14): Follicles mature, estrogen rises
- Ovulatory phase (Day 14-16): Egg is released
- Luteal phase (Days 17-28): Progesterone rises to prepare for possible pregnancy
With PCOS:
- Follicular phase is extended: Follicles develop slowly or incompletely, so it may take weeks or months to mature an egg
- Ovulation may not occur: Follicles develop but don't release an egg (anovulation)
- No luteal phase without ovulation: Without ovulation, progesterone doesn't rise and there's no true luteal phase
- Periods are irregular or absent: May go months without a period, or have unpredictable cycles
- Bleeding can be abnormal: Very light, very heavy, or prolonged
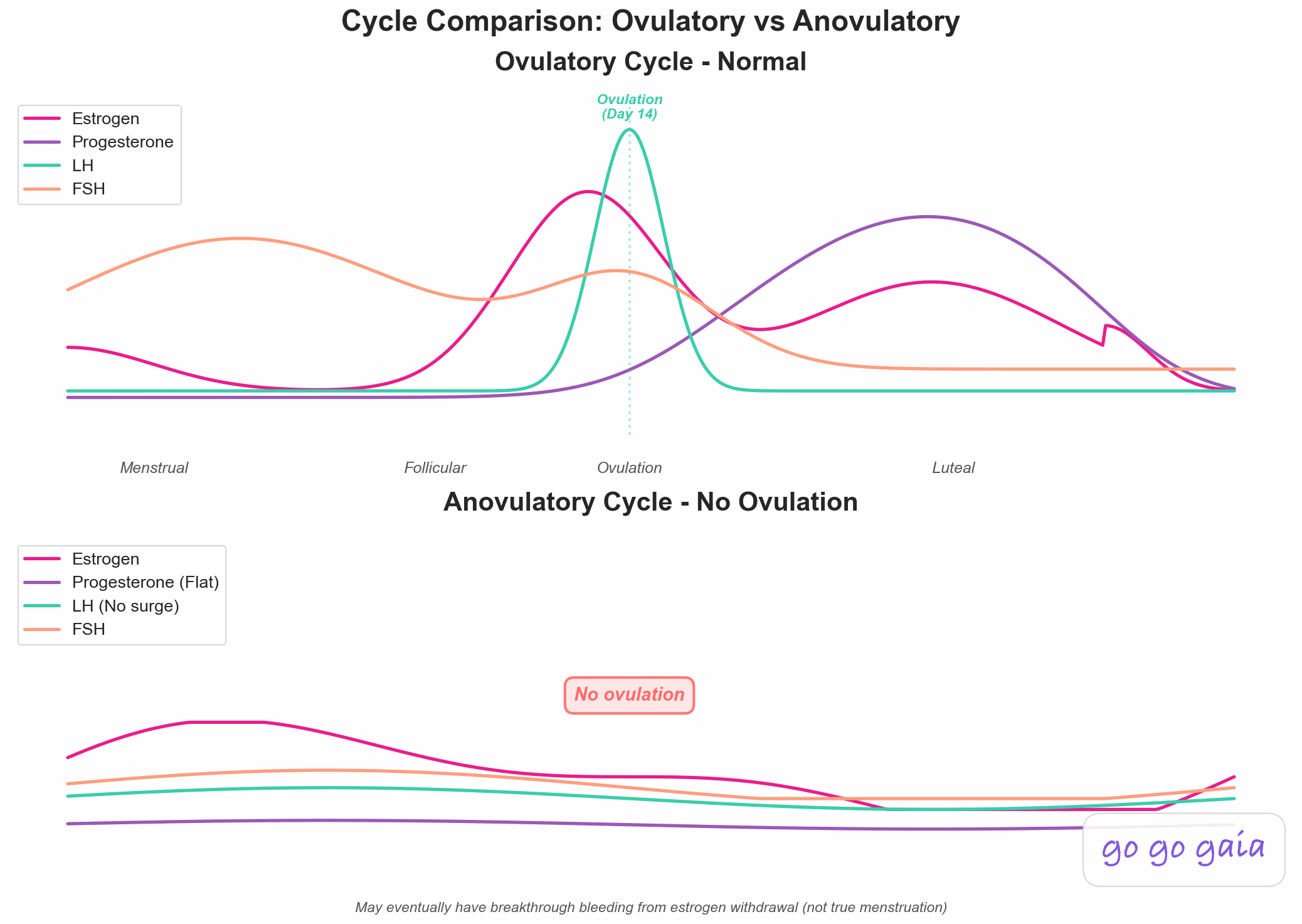
Comparison of normal ovulatory cycle (top) versus anovulatory cycle common in PCOS (bottom)
What This Means for Cycle Syncing
The standard cycle syncing advice (tailoring workouts and nutrition to phases) assumes regular, ovulatory cycles. With PCOS, you can't follow the typical 28-day cycle blueprint.
But that doesn't mean tracking is useless. Far from it! You just need a different approach:
- Track symptoms, not calendar days: Focus on energy, mood, symptoms, cravings (not which "phase" you're in)
- Look for YOUR patterns: You may have more "flat" energy without the typical ups and downs, or you may notice subtle patterns that emerge
- Identify triggers: What makes symptoms better or worse?
- Monitor ovulation signs: Cervical mucus, basal body temperature, ovulation tests to detect IF and WHEN you ovulate
- Track interventions: See what actually improves YOUR symptoms and cycle regularity
Signs Your Cycle is Improving
As treatments work, you may notice:
- Cycles becoming more regular (even if still long)
- Return of ovulation signs (fertile cervical mucus, ovulation pain, thermal shift)
- More predictable energy patterns
- Improved PMS symptoms
- More regular periods
Go Go Gaia adapts to irregular cycles. It doesn't force you into a 28-day mold. Instead, it learns YOUR pattern (even if your pattern is "unpredictable") and helps you spot improvements over time.
Tracking PCOS: What to Monitor
Consistent tracking is one of the most powerful tools for managing PCOS. Here's what to track and why:
Essential Metrics for PCOS
Menstrual Tracking
- Period start and end dates - Establishes cycle length patterns
- Cycle length - Shows if cycles are becoming more regular (a sign treatments are working)
- Flow intensity - Very light or very heavy bleeding can signal issues
- Spotting - Between-period bleeding patterns
Ovulation Signs (If Tracking Fertility)
- Cervical mucus - Egg-white consistency indicates fertile window
- Basal body temperature - Temperature rise confirms ovulation occurred
- Ovulation test results - LH surge predicts ovulation
- Mittelschmerz - One-sided pelvic pain during ovulation
Physical Symptoms
- Acne location and severity - Tracks androgen levels indirectly
- Excess hair growth - Changes very slowly, but important to monitor
- Hair loss or thinning - Track areas and progression
- Skin changes - Acanthosis nigricans, oiliness
- Weight and measurements - If relevant to your management plan
Metabolic Signs
- Energy levels - Rate daily to spot patterns
- Hunger and cravings - Especially carb cravings (indicates blood sugar dysregulation)
- Energy after meals - Crashes suggest insulin issues
- Sleep quality - Poor sleep worsens insulin resistance
Mood and Mental Health
- Anxiety levels - Higher in women with PCOS
- Depression symptoms - More common with PCOS
- Stress levels - Directly impacts symptoms
- Overall wellbeing - General sense of how you're doing
Interventions and Treatments
- Medications - Doses, timing, and consistency
- Supplements - What you're taking and when
- Exercise - Type, duration, intensity, and how you felt
- Diet changes - New eating patterns or foods eliminated
- Stress management practices - Meditation, therapy, etc.
Why Consistent Tracking Matters
Tracking PCOS symptoms consistently for 3-6 months reveals:
- What actually works for YOU - Not generic advice, but personalized insights
- Which symptoms cluster together - Helps identify your PCOS type
- Triggers for symptom flares - Stress, certain foods, lack of sleep
- Progress over time - Changes happen slowly; tracking proves they're happening
- When ovulation returns - Critical for fertility
- Data for your healthcare provider - Makes appointments more productive
How Go Go Gaia Helps with PCOS
.png)
Go Go Gaia's dashboard adapts to irregular cycles and tracks the metrics that matter for PCOS
Managing PCOS requires tracking multiple health metrics and spotting connections between them. Go Go Gaia is specifically designed for this:
Irregular Cycle Adaptation
- Doesn't assume a 28-day cycle
- Adapts to YOUR pattern, no matter how irregular
- Shows cycle length trends over time
- Highlights when cycles are becoming more regular (a sign treatments are working)
- Tracks anovulatory cycles vs. ovulatory cycles
Multi-Symptom Correlation
- Tracks period, symptoms, mood, energy, workouts, nutrition, and medications all in one place
- Identifies which symptoms appear together (your PCOS pattern)
- Shows triggers: "You rate energy as low after eating high-carb meals" or "Stress events correlate with acne flares 3 days later"
- Reveals what improves symptoms: "Your energy improved after starting daily walks"
Healthcare Provider Reports
- Generate detailed reports showing 3-12 months of data
- Cycle lengths and regularity patterns
- Symptom frequency and severity over time
- Response to treatments and interventions
- Speeds up diagnosis and treatment adjustments
AI-Powered PCOS Insights
Ask Gaia questions based on YOUR tracked data:
- "Is my cycle getting more regular?"
- "What foods seem to affect my energy?"
- "Am I ovulating?"
- "Which symptoms have improved since starting metformin?"
- "Should I see my doctor about this?"
All Your Health Data in One Place
- No juggling multiple apps or notebooks
- One-tap logging for quick daily tracking
- Visual dashboards show patterns at a glance
- Reminders help you stay consistent
Living with PCOS: Long-Term Health
PCOS is a lifelong condition, but that doesn't mean a lifetime of suffering. With proper management, you can live a completely healthy, normal life. However, PCOS does increase risk for certain conditions[1] (awareness and prevention are key):
Associated Health Risks
Type 2 Diabetes
Women with PCOS have a significantly higher risk of developing type 2 diabetes, especially if insulin resistance is present. Prevention: Manage blood sugar through diet and exercise, maintain healthy weight, regular screening (fasting glucose and A1c annually or as recommended).
Cardiovascular Disease
PCOS increases risk of high blood pressure, high cholesterol, and heart disease. Prevention: Anti-inflammatory diet, regular exercise, don't smoke, manage weight and blood pressure, regular lipid panel screening.
Endometrial Cancer
Infrequent or absent periods mean the uterine lining doesn't shed regularly, increasing endometrial cancer risk. Prevention: Ensure regular shedding (via natural periods, birth control, or progestin therapy), report any abnormal bleeding to your doctor.
Sleep Apnea
More common in women with PCOS, especially with weight gain. Signs: Loud snoring, gasping during sleep, daytime fatigue. Talk to your doctor if suspected.
Non-Alcoholic Fatty Liver Disease (NAFLD)
Linked to insulin resistance. Prevention: Manage insulin resistance, avoid excessive alcohol, maintain healthy weight.
Mental Health
Women with PCOS have higher rates of anxiety and depression. Support: Therapy, support groups, medication if needed, stress management, self-compassion.
Why This Isn't Scary
Reading this list can feel overwhelming. Here's the truth: These risks are significantly reduced with proper PCOS management.
- Early diagnosis and intervention prevent most complications
- Lifestyle changes dramatically reduce risk
- Regular screening catches issues early when they're most treatable
- Tracking helps you stay on top of your health proactively
- Millions of women with PCOS live long, healthy, fulfilling lives
Knowledge is power. Knowing your risks means you can take action.
Pregnancy with PCOS
PCOS is one of the leading causes of infertility,[6] but most women with PCOS can and do get pregnant, with or without medical help.
Challenges:
- Irregular or absent ovulation makes timing difficult
- May take longer to conceive than women without PCOS
- Higher miscarriage risk, especially in first trimester
- Increased risk of gestational diabetes and preeclampsia during pregnancy
What helps:
- Weight loss (if overweight): Even 5-10% can restore ovulation
- Lifestyle optimization: Diet, exercise, stress management
- Tracking ovulation: Essential for timing intercourse. Use cervical mucus, BBT, ovulation tests
- Metformin: May help restore natural ovulation
- Ovulation induction: Letrozole or Clomid if lifestyle changes insufficient
- IVF: High success rates for women with PCOS
Go Go Gaia's fertility tracking helps you identify your fertile window (even with irregular cycles) by monitoring ovulation signs, giving you the best chance of conception.
PCOS Troubleshooting
"I've tried everything and nothing works"
This is incredibly frustrating. Consider:
- Have you tried consistently for 3-6 months? PCOS changes happen slowly
- Are you tracking to verify what you're trying? Sometimes changes are happening but hard to notice
- Have you had comprehensive blood work recently? Thyroid, vitamin D, insulin, androgens
- Is stress or sleep undermining your efforts?
- Consider seeing an endocrinologist or PCOS specialist for advanced evaluation
"I can't lose weight no matter what I do"
- Weight loss with PCOS is genuinely harder due to insulin resistance. You're not "failing"
- Focus on health improvements beyond weight: energy, mood, cycle regularity, symptom reduction
- Have thyroid function checked (hypothyroidism is common and makes weight loss difficult)
- Consider working with a PCOS-specialized dietitian
- Track non-scale victories: clothing fit, energy levels, blood work improvements
- Some women need medication (metformin, GLP-1 agonists) to help with insulin resistance
"My doctor just says to lose weight"
- If your concerns are dismissed without proper testing, seek a second opinion
- You deserve comprehensive blood work and evaluation regardless of weight
- Being overweight is a symptom of PCOS, not the cause
- Bring tracked data to appointments. Objective evidence is hard to dismiss
- Look for PCOS-informed healthcare providers (endocrinologist, reproductive endocrinologist)
"I have lean PCOS. Do I still need to worry about this?"
- Yes! 20-30% of women with PCOS are normal weight or lean
- You still have hormonal imbalances and health risks
- All the same management strategies apply (except weight loss)
- You may have inflammatory PCOS or post-pill PCOS
- Focus on nutrition quality, exercise, stress management, and regular monitoring
"My periods came back, can I stop treatment?"
- Talk to your doctor before stopping any medications
- PCOS is a lifelong condition. Symptoms can return if lifestyle changes aren't maintained
- Many women need ongoing management, though treatment may evolve over time
- Continue tracking to catch early warning signs if symptoms return
Finding Support and Resources
Healthcare Providers
- Endocrinologist: Hormone specialist, ideal for PCOS management
- Reproductive endocrinologist: If fertility is a concern
- Gynecologist: Familiar with PCOS, can prescribe first-line treatments
- Registered dietitian: Preferably one with PCOS experience for nutrition guidance
- Therapist or counselor: For mental health support
Questions to ask when finding a provider: "How many patients with PCOS do you see?" "What's your approach to PCOS management?" "Do you stay current with PCOS research?"
Online Communities and Support
- r/PCOS: Active Reddit community with 200k+ members sharing experiences and advice
- PCOS Awareness Association: Education and advocacy organization
- PCOS Challenge: Support, resources, and community
- Local support groups: Search for PCOS support groups in your area
Reputable Information Sources
- American College of Obstetricians and Gynecologists (ACOG)
- Endocrine Society Clinical Practice Guidelines
- National Institutes of Health (NIH)
- UpToDate (medical reference used by doctors)
The Bottom Line
PCOS affects 1 in 10 women. You are not alone. It's frustrating, challenging, and often takes years to diagnose. But here's what you need to know:
- PCOS is manageable. You can live a healthy, symptom-controlled life.
- Lifestyle changes are powerful. Often more effective than medication alone.
- Every woman's PCOS is different. What works for someone else may not work for you, and that's okay.
- Tracking changes everything. It reveals YOUR unique PCOS pattern and what actually helps YOUR body.
- You're not "broken." Your body just needs a different approach.
- Most women with PCOS can get pregnant if desired, though it may take time or assistance.
- Progress is slow but real. Give interventions 3-6 months before judging effectiveness.
- You deserve proper diagnosis and care, regardless of weight or appearance.
PCOS is lifelong, not a sprint. Be patient with yourself. Celebrate small victories. Track your progress. Find healthcare providers who listen. Connect with others who understand.
And remember: PCOS doesn't define you. You are so much more than a diagnosis.
Ready to Start Understanding Your PCOS?
Go Go Gaia makes tracking PCOS symptoms effortless with irregular cycle adaptation, multi-symptom correlation, healthcare provider reports, and personalized insights.
Download Go Go Gaia FreeJoin thousands of women taking control of their PCOS with tracking.